Hereditary Hemorrhagic Telangiectasia (HHT) is a multisystemic disease that affect a number of organs. Although the disease can manifest with catastrophic symptoms, diagnosis is not an easy matter. It requires a clinical suspicion due to the atypical and sometimes weakness and/or absence of symptoms, and requires the cooperation of a number of specialties (radiology, cardiology, pulmonary medicine, gastroenterology, ENT).
Definition: What is HHT
HHT involves recurrent epistaxis (nosebleeds), telangiectases, and multi-organ arteriovenous malformations (AVMs).
Original descriptions of familial epistaxis were made by Sutton in 1864 and Babington in 1865. The name Osler-Weber-Rendu originates from the researchers Henri Rendu, William Osler and Frederick Parkers Weber, who contributed in the description and understanding of the disease.
The term Hereditary Hemorrhagic Telangiectasia (HHT) was proposed in 1909 by F.M. Hanes.

Epidemiology
The prevalence of HHT is estimated at 1 in 5,000 to 1 in 10,000 people, depending on geographic region.
Etiology
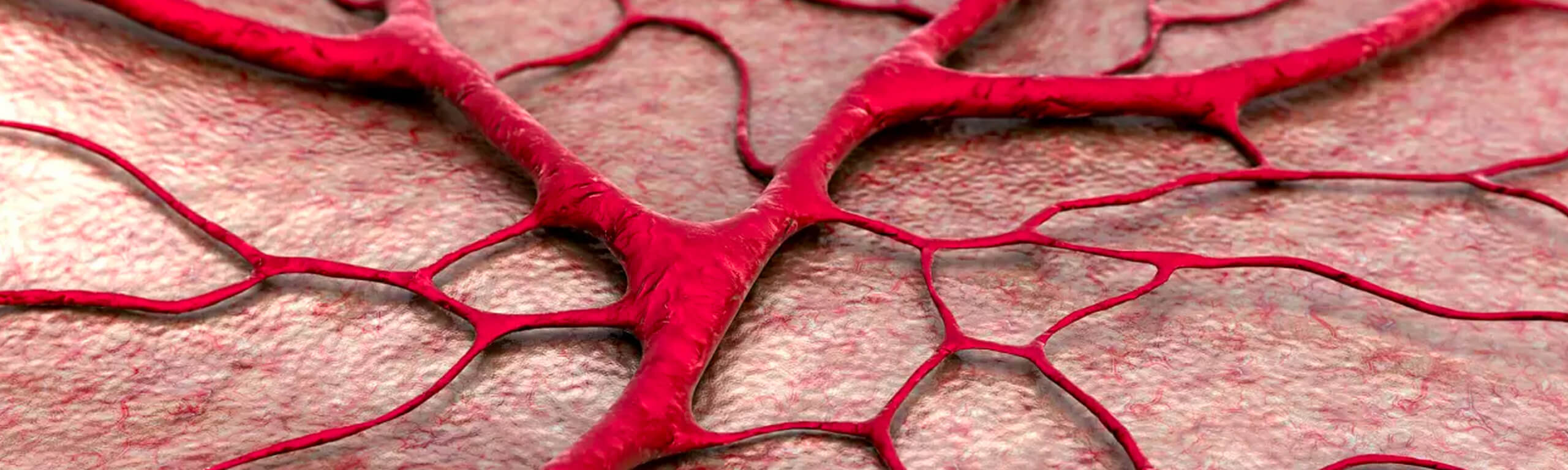
It is an inherited developmental disorder of the vascular system, which is described by an absence of intervening capillaries in the affected areas, resulting in direct connections between arteries and veins.
The small, pink to red, pinpoint to pinhead-size lesions are called telangiectases.
Arteriovenous malformations are larger lesions that are greater than a few millimeters in diameter and sometimes up to several centimeters in diameter.
HHT is inherited in an autosomal dominant manner. Mutations of at least five genetic types are involved in its pathogenesis. However, 85% of all cases are due to the mutations of two genes (ENG-endoglin and ACVRL1/ALK1)
Clinical description of HHT
HHT is a progressively developing disease with a wide range of symptoms, which are related to age, affected organ, and type and extent of the manifestation.
Telangiectases
Telangiectases have been described in 74% of patients, half of whom were under 30 years of age. They develop on the lips, tongue, fingers, skin, nasal, oral and gastric mucosa. Their number increases with age.
Epistaxis and GI bleeding are the most severe manifestations.
- Epistaxis
It is due to telangiectases of the nasal mucosa. Spontaneous night-time nosebleeds are a classic manifestation of the disease. Nasal bleeding is the most common and earliest manifestation of the disease. Onset ranges from infancy to the age of 10. Frequency increases with age. 80-90% will present nosebleeds at the age of 21, while 90-96% of patients will develop recurrent nosebleeds. - Gastrointestinal bleeding
This is the initial symptom in adult patients and usually begins after the age of 40. It can manifest as iron deficiency anemia. Telangiectases may develop anywhere along the GI tract; however, most commonly in the stomach, duodenum and initial segment of the small intestine. On rarer occasions they may be related to AVMs and aneurysms, which are diagnosed with gastrointestinal tree angiographies. - Mucosal telangiectases
These develop in 95% of patients. They typically appear after childhood and increase with age. The percentage of individuals with telangiectases of the hands, face and oral cavity is similar to the percentage with epistaxis, but the age of onset of visible telangiectases is generally 5-30 years later than for epistaxis. Bleeding may occur, but it is rarely of any clinical significance. The main concern of these lesions relates to their appearance.
Arteriovenous Anastomoses Of Visceral Organs
Pulmonary Arteriovenous Malformations (PAVMs)
PAVMs are present in 50% of patients with HHT. Although they are present from childhood, they usually manifest after an individual is in their 3rd decade of life. There are two pathophysiological consequences of PAVMs:
- The presence of a right-to-left blood flow
- The absence of a filtering capillary bed.
Symptoms from the respiratory system
Right-to-left shunting of desaturated venous blood leads to hypoxia and its consequences.
PAVM symptoms may include:
- Breathlessness especially during fatigue
- Platypnea (breathlessness that occurs in the upright position and is relieved with recumbency)
- Orthodeoxia (low concentrations of O2 in the upright position compared to the recumbent position)
- Cyanosis, clubbing and polycythemia polycythemiasecondary to hypoxia
- Neurological symptoms
Shunting of emboli, bacteria and/or air to the circulatory system due to absence of a filtering capillary bed results in the development of paradoxical embolic events (transient ischemic attack, epilepsy) and abscesses in the CNS.
An increased incidence of migraine has also been described in PAVM patients.
Hemoptysis and hemothorax
Bleeding due to the rupture of fragile PAVM vessels to the bronchi and the pleural cavity causes hemoptysis or pneumothorax, fatal hemorrhage. It is rare (<8%) and is mainly associated with gestation.
PAVM is diagnosed using imaging, mainly chest CT. An MRA (Magnetic Resonance Angiography) is useful in the investigation of young patients to avoid radiation exposure. A pulmonary angiogram is required to investigate the vascular architecture of the malformation before embolization.
Hepatic arteriovenous anastomoses
The frequency of hepatic vascular abnormalities was 74% in one study that systematically imaged the liver in HHT patients using CT and 41% in another study using ultrasound examination.
Hepatic venous malformations may be focal, namely in the hepatic artery to hepatic vein, or diffuse. Silent hepatic AVMs occur in more than one in three patients. Hepatic AVMs may manifest in high output cardiac failure, portal hypertension or biliary disease.
Diagnosis is made using CT, MRI, Doppler ultrasound or angiography.
Cerebral Arteriovenous Malformations
Cerebral AVMs occur in 10% of affected individuals. They are usually multiple and silent. They can lead to headache, seizures, ischemia or hemorrhage.
Intracranial hemorrhage secondary to cerebral AVM has been reported as the presenting symptom of HHT in infants and children with HHT. A brain MRI is the most sensitive method for diagnosis.
Complications Of HHT
Pulmonary hypertension
Pulmonary hypertension is another vascular manifestation of HHT. It develops due to a variety of factors including increased cardiac output due to systemic arteriovenous shunting to the liver.
Venous hypertension
HHT patients are at a higher risk of developing venous thromboembolism. Treatment raises red flags due to the use of anticoagulants, which are not recommended in HHT patients.
HHT diagnosis
Clinical diagnosis of HHT is based on the Curacao criteria, which were published in 2000.
These criteria include:
- Epistaxis: spontaneous and recurrent
- Telangiectases: multiple, at characteristic sites (lips, oral cavity, fingers, and nose).
- Visceral AVMs: GI telangiectases (with or without bleeding), pulmonary, hepatic, cerebral and spinal cord AVMs.
- Family history: diagnosis of HHT in a first-degree relative using these criteria.
Treatment of HHT
The treatment of HHT symptoms (epistaxis, GI bleeding, anemia, etc.) is the same as treatment in individuals without HHT. Embolization is used to treat AVMs in target organs (lung, liver, brain).
In recent years, however, drugs, and specifically bevazicumab, a vascular endothelial growth factor (VEGF) antagonist, are being used, which prevent the binding of the VEGF with its receptors, Fit1 (VEGFR1) and KDR (VEGF-2), on the surface of the endothelial cells, thus reducing angiogenesis.
There are many centers of excellence in North America which follow up these patients and numerous published studies with a limited number of patients that show improvement of their symptoms after treatment with the specific drug.
As part of the effort to manage this specific disease, my colleagues and I administer this treatment at Metropolitan Hospital, which is a first for Greece.
We are also in a position to diagnose, treat and follow up patients with all forms and stages of the disease in collaboration with the North American Center of Excellence.
Follow-up of Hereditary Hemorrhagic Telangiectasia
HHT patients must be followed up by a specialized center for life.
Family testing
Upon diagnosis of HHT, first-degree relatives must undergo genetic testing. Particular emphasis is placed on testing relatives for PAVMs due to high familial incidence (>35%).
Prognosis
Facing a high rate of morbidity and death are:
- Pregnant women with HHT due to pulmonary or cerebral hemorrhage or thrombosis.
- Younger patients due to AVM complications related to visceral organs, pulmonary embolism, cerebral hemorrhage and venous thromboembolism.