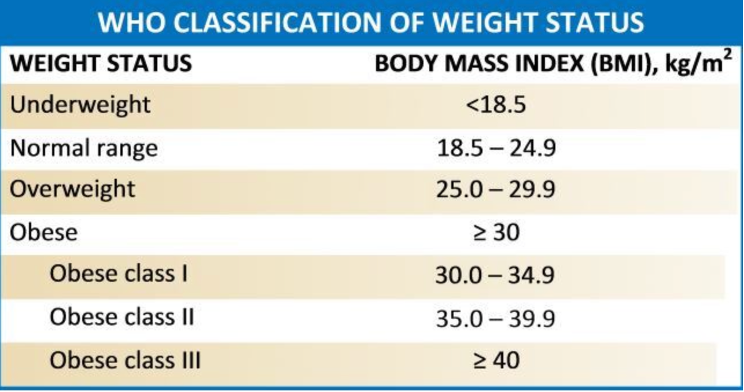
Obesity is a disease recognized by the World Health Organization since 1997 and defined as "abnormal or excessive accumulation of fat that may impair health". It is a real scourge of our society because it is a complex disease that affects millions of people and is currently one of the leading causes of death worldwide. Obesity is assessed by the Body Mass Index (BMI), which is directly correlated with the amount of body fat. According to the World Health Organization (WHO), overweight in adults is defined as presence of a BMI of 25-30 kg/m2 and obesity as presence of a BMI equal to or greater than 30 kg/m2.
What is the definition of severe obesity?
Severe obesity is a very serious disease that has seen an unprecedented spread in the last 30 years, nowadays taking on global epidemic proportions. It is defined as the presence of a BMI greater than 40 kg/m2 with or without comorbidities, or a BMI greater than 35 kg/m2 with at least one obesity-related comorbidity. It is a problem with serious social and psychological dimensions and affects all ages and socio-economic classes. Greece has one of the highest rates of obesity and severe obesity in Europe, both among adults as well as adolescents and children. According to the latest data (year 2022), it is estimated that 37.9% of adults in Greece are overweight, 24.9% are obese, while 41.2% of children aged 10-12 years old are obese or overweight. These rates show the magnitude of severe obesity in our country and cause great concern for the future of our population.
Severe obesity is a chronic multifactorial disease with at least 4 components: genetic, endocrinological, microbiotic and psychological. Behavioral disorders (eating, sedentary life) and discrimination to which these patients are subject are more aggravating factors than real causes, contrary to current prejudices. Therefore, the treatment of severe obesity is difficult because it must be multifactorial and consider the person as a whole.
Which are the obesity-related diseases of a patient with severe obesity?
In our era, for numerous reasons related to eating habits modifications and modern lifestyle, the number of people with higher than normal weight is constantly increasing. People who initially have a normal weight for their age and sex, as they accumulate more and more weight over time, they become initially overweight and then obese. It is now known that being overweight is associated with an increased risk of cancer (e.g. esophagus, colon, rectum, breast, etc.), high blood pressure, cardiovascular diseases, depression, metabolic disorders such as diabetes, osteoarthritis, back pain, gastroesophageal reflux, gallstones, infertility, respiratory disease and sleep disorders. These serious health consequences make obesity a disease that causes premature mortality. All these comorbidities require multifactorial care from different specialties, which is provided at our center.
How can a patient lose weight?
The best way for a patient to lose weight is, without a doubt, proper diet and physical exercise. Unfortunately, in many cases of patients with severe obesity, this is not enough as a sole measure. Scientific studies of the last 10 years have shown that in cases where modification of eating habits, physical exercise and medication are fruitless, then the only substantial and effective solution against severe obesity is surgical treatment. Especially for certain subgroups of obese patients, such as severely obese patients with type II diabetes mellitus, surgery is not only indicated but recommended as first-line treatment.
Surgery for severe obesity & metabolic diseases
Metabolic and bariatric surgery is the surgical specialty that aims to help a patient get rid of excess weight and the related comorbidities caused by it. In recent years, the increased understanding of the mechanisms around severe obesity and human metabolism as well as the progress in various fields of medicine have resulted in not only having patients' weight loss as a goal after bariatric surgery, but also treating the metabolic syndrome from which the great majority of obese patients suffer (hence the term "Metabolic Surgery").
What are the existing surgical "solutions"?
A significant number of scientific studies have shown that surgical treatment of severe obesity is effective in losing weight, improving or treating comorbidities, and reducing the number of deaths related to the disease. Bariatric surgery is now extremely popular around the world (e.g. in the USA and France the number of annual operations has tripled since 2006).
The significant increase of bariatric surgery procedures is related to the current obesity pandemic, the proven effectiveness bariatric surgery for weight loss and treatment of obesity-related comorbidities, as well as the development of minimally invasive or laparoscopic surgery. Indeed, laparoscopic surgery (surgery through small incisions of 5 or 10 mm) has been one of the greatest innovations in the field of bariatric surgery since it has allowed treatment of patients who were considered impossible or too risky for their health to undergo surgery, reducing postoperative pain and offering them a faster return to their activities, with greatly improved aesthetic results. At the same time, in this way the risk of postoperative complications is also reduced. Thus, worldwide as well as in our center, all operations and re-operations of bariatric surgery are performed laparoscopically.
The laparoscopic approach should routinely be the first choice for patients with severe obesity undergoing surgery, since laparoscopy allows excellent view of the surgical field and the entire intra-abdominal region, preservation of the abdominal wall and reduction of postoperative complications (especially respiratory and thromboembolic complications). Today, two are the most popular metabolic and bariatric procedures: sleeve gastrectomy and gastric bypass.
Sleeve gastrectomy
Sleeve Gastrectomy is a relatively simple surgical procedure involving the resection of 2/3 of the stomach volume (fundus and body of the stomach), forming a gastric tube as an extension of the esophagus, which expands into the antrum. The removal of the fundus and the largest part of the body of the stomach result in a drastic reduction in gastric capacity, in a way that the feeling of satiety and fullness occurs sooner with much less quantity of food (restrictive effect). In addition, in the fundus of the stomach (which is removed during the operation), the hormone ghrelin is produced by some specialized cells, which is considered by newer studies to be the most active neuroendocrine factor that regulates appetite. In particular, when the stomach remains empty, the levels of ghrelin in the blood increase and give the message to the part of the brain that regulates appetite that we are hungry. Both the reduced capacity of the remaining stomach and the reduction of ghrelin levels due to fundus removal are the main mechanisms of action of sleeve gastrectomy.
Sleeve gastrectomy is technically easy when performed by experienced bariatric surgeons. It is performed laparoscopically in about 1 hour and requires a 1- to 3-day hospital stay. Typically, the patient is fed liquids from the first day after surgery while being put on a liquid food diet for two weeks, then a soft food (mixed, mushy) diet for another two weeks, and then eating several small regular meals per day, continuing his life normally. Most patients who undergo a sleeve gastrectomy lose 70%-100% of excess weight within 12 months, and maintain their results long after or for life. An impressive improvement of their comorbidities is also observed: most patients taking medication for hypertension and/or diabetes mellitus are immediately able to reduce their doses or stop medication, sleep apnea is completely cured in over 70% of patients, dyslipidemia is cured in over 50% of patients, etc. To obtain an optimal result, close cooperation of the patient with the team that monitors him postoperatively is necessary, while physical exercise is mandatory.
Roux-en-Y gastric bypass
Roux-en-Y gastric bypass is a surgical procedure that leads to significant weight loss through restrictive and malabsorptive effects ("mixed" type procedure). First, a very small gastric pouch is created in the upper part of the stomach (restrictive effect). This pouch is directly connected to the small intestine (at 1.5 meters from its beginning) so the food after swallowing does not pass through the rest of the stomach, the duodenum and a part of the small intestine, moving faster to the peripheral intestine (malabsorptive effect). For this reason, the operation was called gastric bypass. This method combines restriction of the food that the patient can consume, modified secretion of digestive tract hormones and reduction of appetite.
Roux-en-Y gastric bypass is a technically more difficult operation than sleeve gastrectomy and should be performed by experienced bariatric surgeons. It is performed laparoscopically, takes about 1.5 hours and requires 2 to 3 days of hospitalization. Patients who undergo it lose weight quickly and can maintain their good results for life (if they are careful postoperatively). Due to the malabsorption caused, patients develop deficiency of some vitamins and/or elements and need to take nutritional supplements for life. For these reasons, this operation is mainly recommended for patients with very important excess weight, those with a serious problem of type II diabetes mellitus that cannot be controlled with medication, as well as for patients who have undergone bariatric surgery in the past and were not able to maintain their weight at a low level or improve their comorbidities. Here again, close cooperation of the patient with the team that monitors him postoperatively as well as physical exercise are necessary for an optimal result after Roux-en-Y gastric bypass.
Other techniques
There are other less common bariatric surgery techniques such as one-anastomosis gastric bypass (mini-bypass), biliopancreatic diversion, SADI-S technique or Bariclip placement that can be recommended to patients on a case-by-case basis. The placement of an adjustable gastric band is a method that is progressively abandoned due to unsatisfactory long-term results and complications related to the intra-abdominal position of the band (slippage, gastric obstruction, gastric perforation, etc.). A large number of patients who had previously a gastric band placed and wish to have it removed were treated successfully in our center, with the removal being performed laparoscopically in all cases. Techniques such as gastric plication, gastric botox or gastric balloon are not applied in our center since numerous international scientific studies have clearly demonstrated their ineffectiveness in patients with obesity.
The Department of Metabolic & Bariatric Surgery
At the Department of Metabolic & Bariatric Surgery of Metropolitan Hospital we follow the international current practices regarding the treatment of overweight patients and obesity. Thus, we offer a multifactorial approach in combination with collaboration with specialized scientists, aiming at obesity prevention and loss of excess weight of our patients. Particularly important is the first stage of care, which must include the release of guilt. Indeed, the obese patient should not be held solely responsible for his condition. Unfortunately, today many obese patients are excluded from society, struggling with "fat racism or chondrophobia". Our center, under the direction of Dr. Panagiotis Lainas, offers to patients a complete interdisciplinary follow-up (medical, metabolic, surgical, nutritional-dietological, psychological, etc.). This includes, for cases where surgery is indicated, preoperative preparation, surgical management on a case-by-case basis and lifelong postoperative monitoring
Dr. Panagiotis Lainas (MD, MSc, MSurg, PhD) is the Head of the Department of Metabolic & Bariatric Surgery at Metropolitan Hospital. He is member of the Board of the Hellenic Society of Bariatric Surgery as well as member of the Board of Young-IFSO Europe. He graduated from the Medical School of the University of Crete and obtained a master's degree and a Ph.D. in Surgical Sciences from the University of Paris-Saclay (Paris, France). He completed his training in minimally invasive general surgery and bariatric surgery at Antoine-Béclère, Cochin and Institut Montsouris Hospitals in Paris (France). He has performed more than 1100 metabolic and bariatric surgeries to date and is the author of numerous scientific publications (121 publications, 2438 times cited, H-index = 24) as well as international congress presentations in the fields of minimally invasive and bariatric surgery.