A team of specialized physicians with extensive experience and the suitable equipment
The Metropolitan Hospital Neurooncology Department has been established to meet the needs of patients with benign or malignant tumors in the central nervous system, i.e. the brain and spinal cord. This is a multidisciplinary team (Neurosurgery, Neuroradiology, Oncology and Radiation Therapy), which aims at providing the best possible and scientifically sound treatment for these complex problems. The oncology multidisciplinary team meets on a weekly basis to discuss and review individual patient care plans.
The team’s objective and goal is to provide services to neurooncology patients that are in line with the best specialized centers abroad.
DEPARTMENT OF NEUROSURGERY
The neurosurgery team of the Neurooncology Department consists of specialized physicians with years of experience in treating neurooncology cases of every complexity in foreign centers. The advanced equipment at Metropolitan Hospital (latest-generation surgical microscope, intraoperative CT scanner, neuronavigator, neuromonitoring systems) allow physicians to provide unique services in Greece.
The neurosurgery team handles the following cases
- Benign and malignant gliomas
- Skull base tumors (meningiomas, acoustic neuromas, craniopharyngiomas, pituitary and sella turcica tumors)
- Spinal cord tumors (ependymomas, gliomas)
- Metastatic brain and spinal tumors

TECHNIQUES EXCLUSIVE TO METROPOLITAN HOSPITAL
- Brain tumor resection in difficult regions while the patient is alert (awake craniotomy)
- Resection of central nervous system tumors under neuromonitoring for the best possible functional result
- Minimally invasive neuronavigation guided access
- Application of the ALA technique and intraoperative imaging using a CT scanner for maximal possible resection of malignant gliomas (glioblastomas)
- Intraoperative chemotherapy
- Endoscopic surgery of abdominal tumors
- O-arm (intraoperative CT imaging system)

RADIATION ONCOLOGY CENTER
Customized, modern and effective treatment
As soon as you visit the Metropolitan Hospital Radiation Oncology Center, you will be approached by a dedicated team of specialists, who will tailor the treatment to your individual needs. Other than Radiation Oncologists, this specialized team includes the Medical Physics Department, which consists of radiophysicists who specialize in the latest radiation therapy technologies, radiologic technologists, nursing and secretarial staff.
The close collaboration with other medical specialties that are involved in the treatment of central nervous system tumors (Neurosurgeons, Neurologists, Medical Oncologists, Neuroradiologists and Anatomic Pathologists) ensures customized, contemporary and effective treatment. The state-of-the-art radiotherapy techniques that are administered by the doctors from their training in centers of excellence in Europe and the USA ensure highly accurate and targeted tumor treatment, by delivering the maximum radiation dose possible, with the least damage to healthy cells.
Radiation therapy and central nervous system tumors
Radiation therapy uses high-energy X-rays to kill cancer cells. Radiation passes through the body and is able to treat tumors in areas of the brain that are surgically inaccessible. Radiation therapy can either be used alone as primary treatment, usually for patients that are not candidates for surgery, or following the surgical resection of a tumor in order to help destroy tumor cells and to prevent them from returning. It is a treatment of choice for many central nervous system tumors (benign or malignant) and tumors originating from other organs (brain metastases). Lastly, it can be administered to reduce neurological symptoms.

STATE-OF-THE-ART RADIATION TREATMENT FOR CENTRAL NERVOUS SYSTEM TUMORS
Intensity Modulated Radiotherapy – IMRT
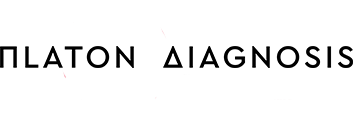
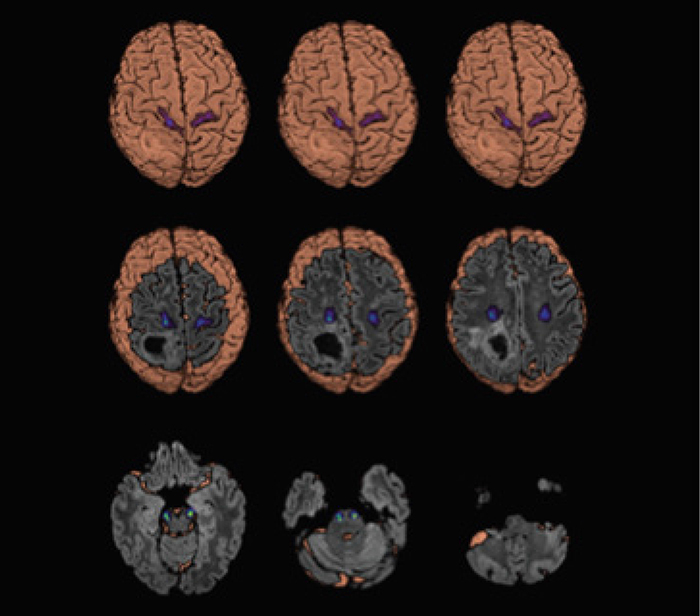
Intensity Modulated Radiotherapy (IMRT) is an advanced type of high-precision and targeted radiation. It is the next generation of three-dimensional conformal radiation therapy (3D-CRT). Contrary to IMRT, 3D-CRT is used in most radiation therapy centers throughout Greece. As evident (Image 1), IMRT further improves the possibility of adjusting the high radiation doses to the shape of the tumor (green and red areas), thus reducing the burden received by the normal tissues and sensitive structures (blue areas).
IMRT allows radiation oncologists to deliver adequate doses to tumors located very close to critical central nervous system structures, such as the optic nerves, the optic chiasm, the brain stem, etc. Without IMRT, these tumors would not have been able to receive the necessary radiation dose, thus compromising chances of recovery.
STEREOTACTIC RADIOSURGERY (SRS) AND STEREOTACTIC RADIATION THERAPY (SRT)
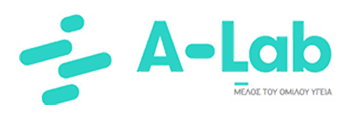
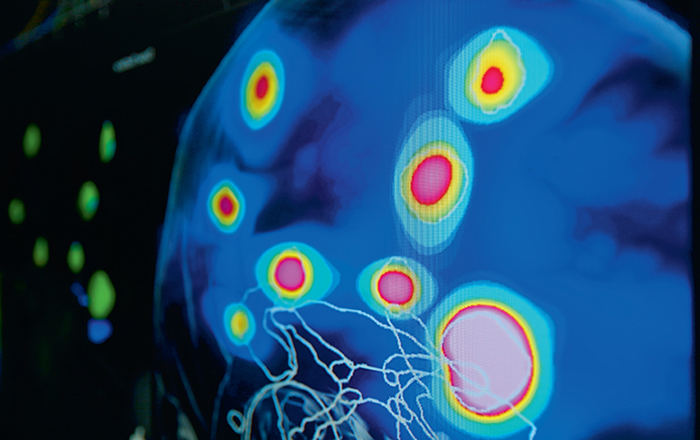
Non-invasive radiation techniques to the treatment of brain tumors and function disorders (Image 2)
SRS and SRT have the following key features:
- Very high accuracy (1-2 mm).
- Very high conformity, with sharp dose decrease on the border of the targeted tumor, leading to the least possible irradiation of the surrounding normal tissue.
- Delivery of very high radiation dose with completion of the treatment in 1 to 5 sessions (Stereotactic Radiosurgery - SRS). SRS is an excellent alternative to interventional surgery, especially when patients cannot undergo surgery or in cases of inoperable tumors and intracranial abnormalities.
SRS is indicated for:
1. Benign and malignant brain tumors:
- Primary malignant brain tumors
- Brain metastases
- Acoustic neuroma
- Meningioma
- Pituitary adenoma (recurrence or residual disease)
- Eye tumors
- Skull base tumors
- Hemangiomas
- Craniopharyngiomas
2. Vascular disorders:
- Arteriovenous malformations
3. Functional abnormalities:
- Trigeminal neuralgia
- Epilepsy
- Parkinson’s disease
MRI
NEURORADIOLOGY & ADVANCED ONCOLOGIC MRI DEPARTMENT
The Metropolitan Hospital leading Neuroradiology & Advanced Oncologic MRI Department implements the most advanced functional/multiparametric MRI techniques. These exams offer the best imaging of the body’s anatomy and the functional study of many organs, providing answers to the most complex diagnostic problems. Specific MRI techniques allow the evaluation of many functional parameters, such as mapping functionally related regions, metabolic activity and microvascular bleeding of the brain.
The aim is the ultra-modern imaging of the central nervous system and other anatomic regions with multiple applications in oncology (diagnosis, preoperative and radiation therapy planning, follow-up of the therapeutic result) and applications in many other diseases of the brain, spine and trachea. The data received from the functional imaging techniques significantly increase diagnostic accuracy in terms of identifying and characterizing the lesion.
They contribute in the appropriate choice of treatment and in the follow-up of the therapeutic result. In addition, the data of the non-invasive mapping of the functionally related regions (e.g. motor or speech cortical areas, pyramidal pathway) are incorporated into neuronavigation systems, in order for the neurosurgeon to choose the most suitable access during surgery and avoid the creation of a permanent neurological deficit (e.g. damage to motor or speech cortical areas would result in paresis or aphasia). The techniques are applied at our Department for diagnostic and research purposes.
MULTIPARAMETRIC | FUNCTIONAL MAGNETIC RESONANCE IMAGING
The multiparametric / functional imaging techniques performed at our Department include:
- Spectroscopy
- Perfusion DSC/DCE
- Diffusion Tensor Imaging (DTI))
- tractography
- Diffusion DWI/IVIM, functional MRI
- CSF Flow Study
- Time Resolved 4D Contrast Enhanced MRA
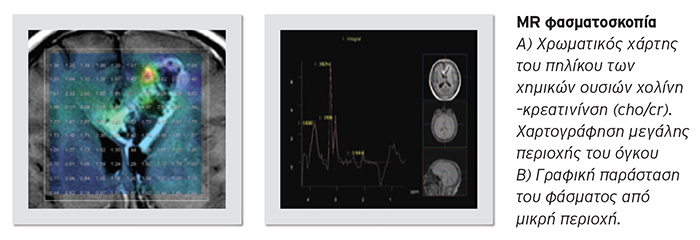
PERFUSION
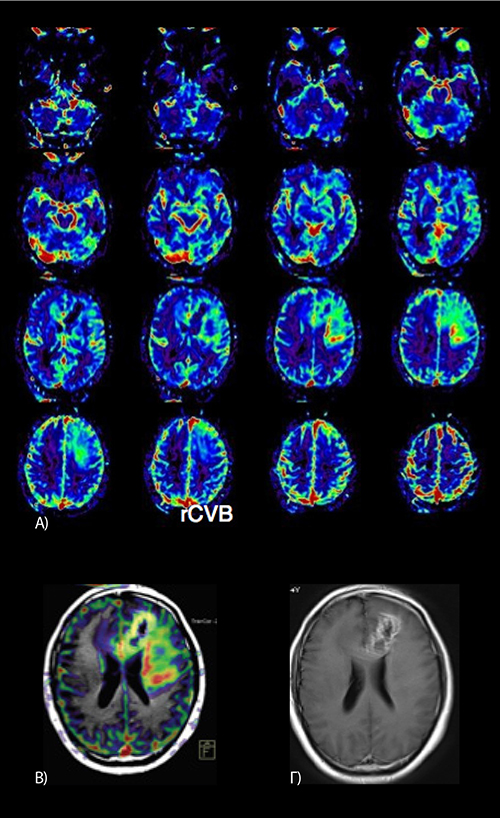
Dynamic study of first pass perfusion (DCE/DSC techniques): It is a dynamic study of the perfusion of an organ at small vessel (capillaries) level. It identifies areas with pathologic perfusion. In neurooncology it identifies perfusion of a tumor with greater accuracy than traditional MRI and helps in the identification of tumors (high/low perfusion), the assessment of their aggressiveness, the size of the tumor and the choice of the most suitable treatment, as well as the assessment of its position for biopsy or radiation treatment planning, and follow-up of the treatment result.
DIFFUSION TENSOR IMAGING (DTI)
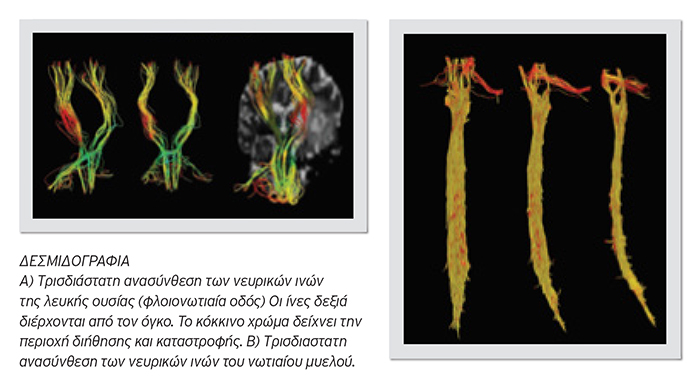
![]()
FUNCTIONAL MRI
Functional MRI is a modern, non-invasive procedure using MRI technology in which we stimulate and then take images of functional regions of the cerebral cortex, such as the motor and speech cortical areas. It is mainly performed prior to surgery as a mapping method, so the neurosurgeon may select the most suitable access and avoid the functional cortical areas, avoiding the creation of permanent damage to the patient, such as paresis or aphasia. Depending on the area of the brain that needs to be depicted, during the exam, patients are asked to execute a series of simple commands, e.g. finger movement at regular intervals when examining the motor cortex.

CLOSE COLLABORATION
According to international standards, our Department is in close collaboration with our Hospital’s Neurological, Neurosurgical, Surgical, Medical Oncology, Radiation Oncology and MRI-Advanced Imaging Departments. The imaging that is performed by our Department enriches the respective clinical information at the weekly Oncology and Neurosurgery Meetings, so that doctors are able to arrive at a diagnostic and therapeutic result that is customized for each patient.
NEUROONCOLOGY CENTER
CALL DAILY 8:00-16:00 ON:
+302104809150, +302104809000 for the Neurooncology Department
9 Ethnarchou Makariou & E. Venizelou Streets, 18547 Neo Faliro