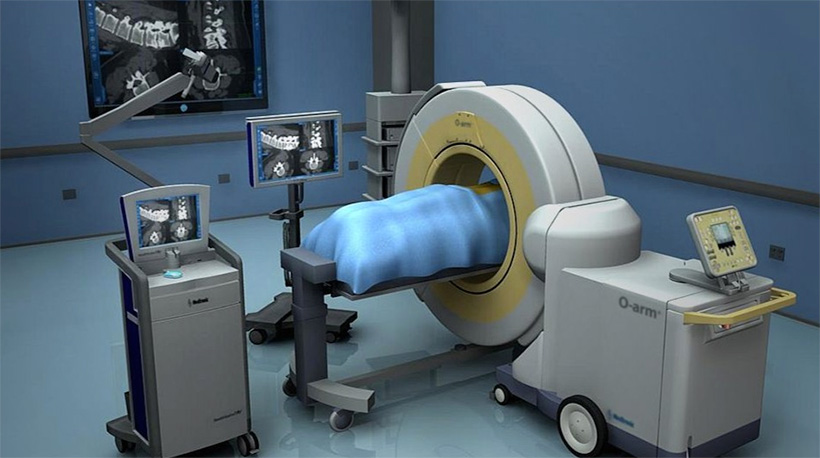
The world of surgery is changing with this new innovative intraoperative imaging system, which is considered a landmark in modern medicine.
The fully portable O-arm CT system is a multi-dimensional platform already used by major surgical centers worldwide. It constitutes a milestone in surgical imaging. Combined with a surgical navigation system, it is the only device that can offer surgeons 100% accuracy for detecting and managing even the most sensitive lesions.
The extreme accuracy of this system allows performing surgical procedures even in the most anatomically dangerous areas, limiting the risk of medical errors. In this way, very delicate, or previously inoperable traumatic brain surgeries to remove tumors in the brain and spinal cord, musculoskeletal pelvis and limb, or other sensitive spinal surgeries, are performed using this innovative technology, for maximum safety and efficiency. The unique O-arm features have resulted in a dramatic reduction in surgical time (up to 50%), which renders surgery an option even in cases of high-risk patients.

At the same time, in addition to the increase in surgical indications, the O-arm can depict three-dimensional internal organs of the body during surgery, eliminating intraoperative risk, while increasing the life expectancy of patients.
HOW THE SYSTEM WORKS
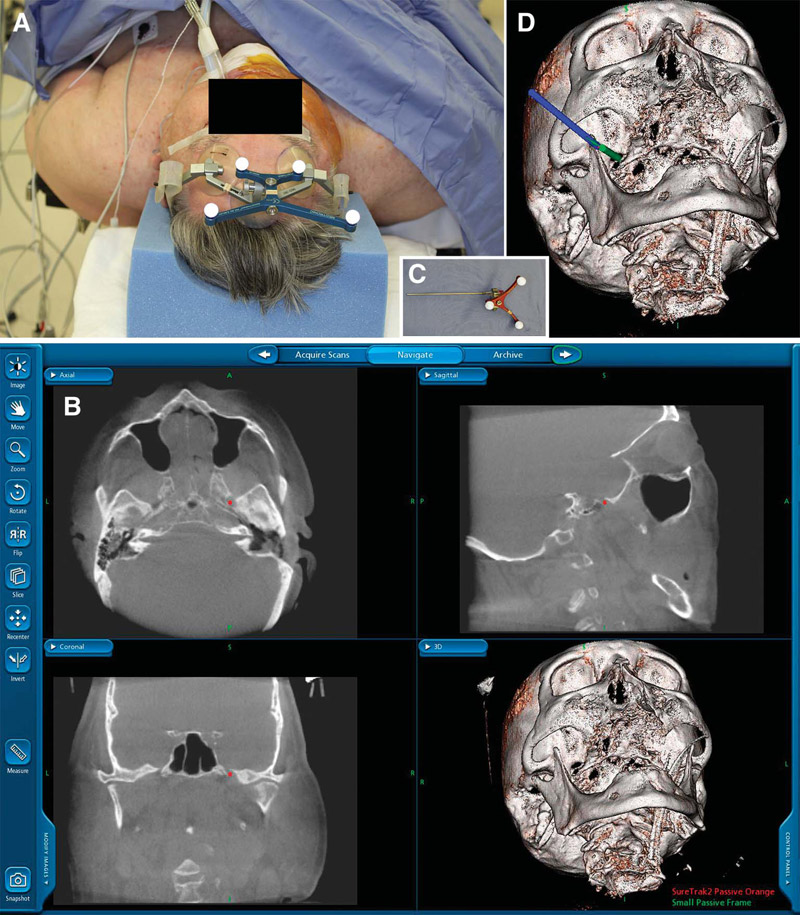
The modus operandi of the system is as follows: Similarly to how satellites detect the position of the GPS unit in our car and our navigation system displays the car's position on a map, a camera inside the operating room detects the position of the surgical instruments. This position appears on the system screen in real time, in direct relation to the actual anatomy of the patient (optical detection technology).
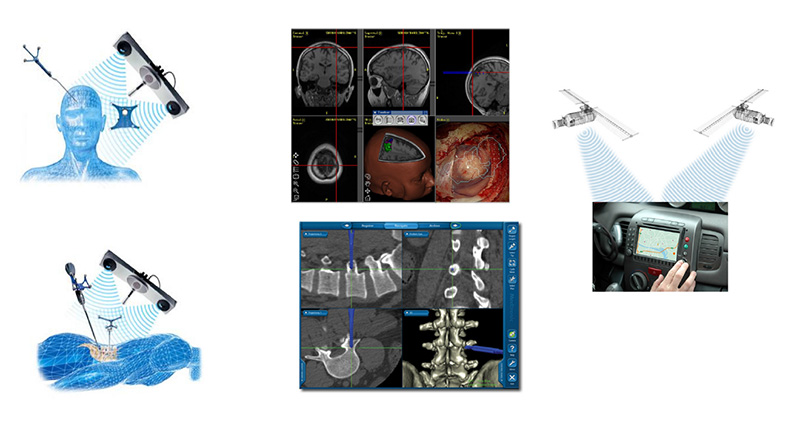
The camera is replaced by a transmitter. The transmitter produces an electromagnetic field around the patient and anything that enters the field is automatically detected by the system (electromagnetic detection technology). Microscopic sensors fitted on the surgeon's tools are detected and pinpointed within the field. This provide the surgeon with constant and highly accurate information about the location of their instruments and the anatomy of the patient.
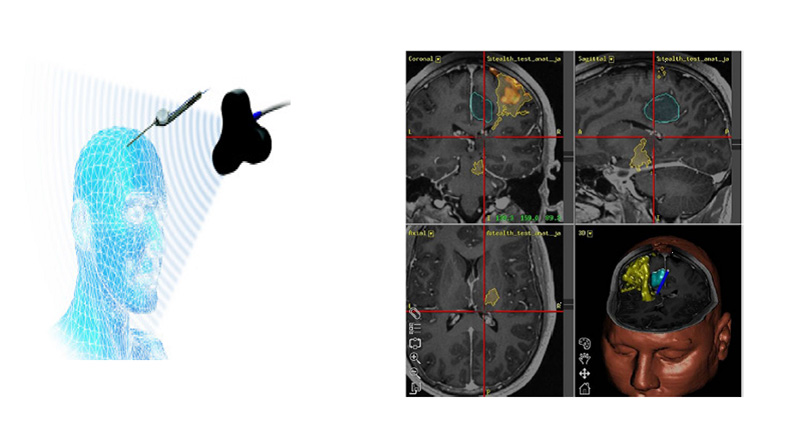
Surgical navigation systems are located inside the surgical room and use either optical or electromagnetic detection technology. They consist of a dedicated camera or transmitter, a computer unit equipped with appropriate software, a screen and special navigation tools, as well as adapters for the detection of common surgical tools by the system.
The special transmitter camera detects and locates the position of the moving tools, crosschecking the corresponding signals (ball reflection in optical technology, electromagnetic field signal). The computer unit receives these signals and their position is displayed on the system screen, on a corresponding map, which is an MRI or CT image or a combination of both, or even other imaging tests.
MAIN APPLICATIONS
The new surgical navigation systems provide a comprehensive methodology for imaging tests (MRI, CT, MRA, axial angiography, ultrasound), preoperative surgical planning, intraoperative navigation and postoperative data archiving. Surgical navigation is mainly used in Neurosurgery, Orthopedics and Otolaryngology.
Modern surgical navigation technology has contributed significantly in the advancement of Neurosurgery and has been internationally established as the method of choice for cranial surgery, replacing older stereotactic methods using a frame.
The main applications in Neurosurgery include:
- Removal of brain and spinal cord tumors (selection of craniotomy and surgical approach/access, detection and localization of tumor)
- Biopsy and catheter placement
- Functional neurosurgery (electrode placement for deep brain stimulation)
- Spinal surgery
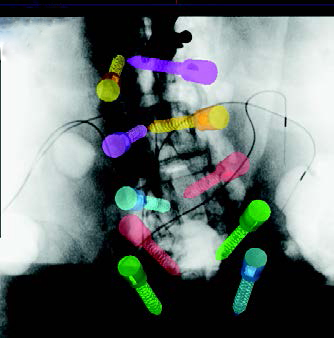
The use of surgical navigation has been developing rapidly in recent years in spinal surgery, as it provides three-dimensional imaging of the anatomies intraoperatively and also allows the detection of the exact location of the tools and implants (screws) in relation to the particular anatomy. Therefore, it allows detailed planning of surgical access, as well as visualization of real-time screw access.

In addition, intraoperative navigation has been recently used in musculoskeletal tumor surgery. In several cases, navigation was used for transcutaneous osteoid osteoma or metastatic lesion ablation, in combination with osteoplasty.
ADVANTAGES OF INTRAOPERATIVE NAVIGATION
The main feature of surgical navigation is that it provides surgeons with more accurate real-time information in the operating room, by depicting the anatomy and the tools in multiple views (axially, anteriorly-posteriorly, laterally) or three-dimensionally.
This information can ultimately provide:
- Greater precision and efficiency of the procedure: For example, during transpedicular screw placement procedures in vertebral arches in posterior scoliosis surgery, there was a significant reduction in the incidence of screw misalignment to 1.8% using navigation, versus 11% observed in cases where only radiographic devices were used.
- Reduced surgical time: In lumbar vertebrae open femoral interventions, it was observed that in the cases where intraoperative navigation was used, the total duration of surgery was reduced by an average of 40 minutes compared to cases where only fluoroscopy devices were used.
- Reduced exposure to radioactivity during spinal surgeries: In transpedicular screw placement procedures, a 70% reduction in radioactivity exposure was observed (from 11.5 seconds for 2 screws per vertebra level using only fluoroscopy devices to 3.5 seconds using navigation).
- Greater sense of security for the surgeon during surgery: Surgical navigation can confirm the surgeon's judgment and the decisions they previously took based only on knowledge of the human anatomy.
- Reduced patient hospitalization time.

With regard to spinal surgery, in practice, the O-arm clearly depicts the difficult and often absurd anatomy of the spine to the surgeon, thanks to the projection of the area in 3 levels in real time. So the use of the O-arm eliminates possible technical difficulties in these interventions.
The most difficult and time-consuming part of the operation can now be accurately predicted, which may reduce required surgery time to as much as 1/3. This offers the option of safe intervention for patients previously considered high risk, as well as reduction of morbidity in these interventions.
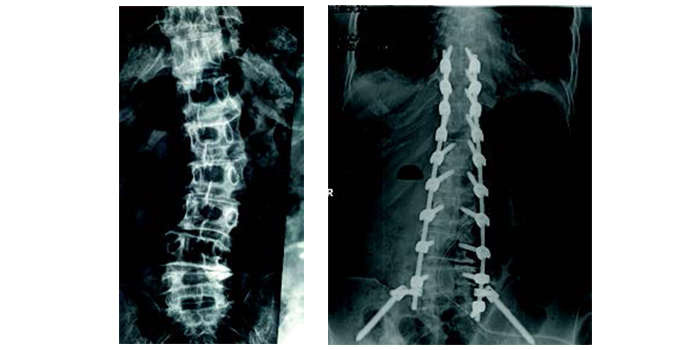
For the same reasons, as complete imaging of the anatomy is now possible, vertebrae which were often overlooked owing to their anatomical difficulty can be treated more easily and there is no need for less effective techniques. This way, all vertebrae are now included in spondylodesis with the use of compression bolts, with an apparently excellent end result for the patient.
In addition, patients often fear paralysis after spinal surgery. Now, insecurity about the nervous tissue and the fear of surgeons and patients of some kind of paralysis is indeed eliminated.
Thanks to the reduced procedure time and the possible complications of the nervous tissue, it is possible to achieve shorter anesthesia time, less blood loss, fewer transfusions, less exposure to infections, shorter stay in the Intensive Care Unit after surgery and significant stress reduction for the patient in general, resulting in less morbidity than non-surgical problems.
SCOLIOSIS AND KYPHOSIS
For the first time in Greece, in June 2016, Metropolitan Hospital successfully implemented the intraoperative 3D imaging / surgical navigation system in children with adolescent scoliosis. The surgical navigation system makes it possible to place the implants in real time as accurately as a CT scanner. This kind of precision eliminates the possibility of medical error and permanent neurological damage, while providing an excellent aesthetic result, which is particularly important for girls suffering from scoliosis. The surgical navigation system is now used by our team on all children and adults with kyphosis or scoliosis.
Scoliosis is characterized by a twisting of the spine. It is a condition that affects children, teenagers and adults of both sexes. Idiopathic scoliosis is the most common form of scoliosis, affecting about 2% of the world population. Kyphosis is an increase in the normal chest curve or a decrease in the normal spine curve. It usually affects older people with osteoporosis, but also teenagers.
Symptoms:
The parents of a child or an adolescent may suspect scoliosis when one shoulder looks higher than the other or the pelvis appears oblique. Observe the child's back for some deformation, usually in the form of the letter "S" or "C".

- In teenagers with back pain and kyphosis, Scheuermann’s disease should be excluded.
- In adults, the gradual displacement of the body to the right or left should give rise to suspicion of scoliosis, especially if it is accompanied by back pain.
Adult kyphosis can be easily identified by a growing hump on the back and the patient's need to walk with bent knees. Back pain is almost always present.
TREATMENT OF SCOLIOSIS / KYPHOSIS
The treatment of vertebral deformities includes 3 aspects:
Monitoring
Every child and teenager with small scoliosis or kyphosis should be monitored at regular intervals for possible deterioration as their body develops. All adults with scoliosis or kyphosis should be monitored for possible deterioration if scoliosis or kyphosis are not accompanied by neurological problems; if they are, immediate treatment is needed. At the initial stage, the role of targeted physiotherapy and medicines is essential for the reduction of pain.
Braces
In children and adolescents with moderate scoliosis, the latest data and advances in synthetic material technology have enabled the creation of lighter and more elegant braces that are more easily accepted by the child. Their role is limited in stopping the deterioration of the curve. Their application time should not exceed 18 hours a day. In adolescents with Scheuermann's disease, the use of an appropriate brace can help in stopping deterioration of the condition, in controlling the pain, and in some cases in fully correcting the kyphosis. Unfortunately, in adults with scoliosis or kyphosis, braces are not as effective as in children and adolescents, whose body is still growing.
Surgical alternatives
For children and adolescents, scoliosis surgery is proposed for curves that have surpassed 45 degrees. If scoliosis cases of such magnitude are left without surgical treatment, they will continue to deteriorate even after skeletal maturation has occurred, resulting in chronic pain, respiratory dysfunction and the psychosocial effects of this distortion, especially for girls. Unfortunately, when scoliosis exceeds 45 degrees, the braces are no longer effective in preventing the deterioration of the deformation. In a teenager suffering from Scheuermann’s kyphosis, if it continues to evolve reaching or exceeding 70 degrees despite the use of a brace and the child complains of persistent pain, surgery should be the treatment of choice.
The treatment of adult kyphosis is usually surgical. Percutaneous and non-surgical interventions, such as kyphoplasty, can help correct kyphosis and the accompanying pain of a recent osteoporotic fracture. Adult scoliosis should be surgically corrected when combined with back or leg pain that restricts daily activities and reduces the quality of life.
SPINAL SURGERY CENTER
DAILY 9:00-16:00 TELEPHONE
+302104809150, +302104809000 for the Spine Surgery Center.
9 Ethnarchou Makariou & E. Venizelou Streets, 18547 Neo Faliro