A remarkable breakthrough in interventional cardiology is the development and clinical application of Transcatheter Aortic Valve Implantation (TAVI) for patients with severe aortic stenosis.
This pioneering technique offers a new horizon as an alternative to surgical valve replacement for patients at high surgical risk.
The bioprosthetic valve, mounted on a special catheter, is advanced through the femoral artery—or, less commonly, through the subclavian artery—and positioned in place of the diseased aortic valve, without the need for extracorporeal circulation.
Our experience with procedures performed at the Metropolitan Hospital has demonstrated that the method is both safe and highly effective, with patients typically discharged within 3–4 days of hospitalization.
Additionally, Metropolitan Hospital also performs catheter ablation procedures for the treatment of complex cardiac arrhythmias, utilizing advanced technology systems with real-time color three-dimensional mapping of the cardiac chambers. This enables precise identification of the arrhythmogenic focus, ensuring successful ablation.
Furthermore, the application of cardiac resynchronization therapy, achieved through pacing of the left ventricle, contributes significantly to the improvement of cardiac function in patients with heart failure.
TAVI or TAVR: Transcatheter Aortic Valve Replacement
Aortic Valve Stenosis
Aortic valve stenosis is the most common valvular heart disease among adults in developed societies. It is estimated that 2–7% of the population over the age of 65 suffers from this condition.
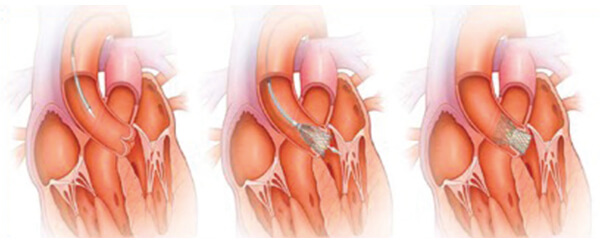
Aortic stenosis is caused by thickening, hardening, and calcification of the valve leaflets, leading to a progressive narrowing of the effective valve orifice. As a result, the heart’s ability to pump the required amount of blood into the circulation becomes severely limited, reducing the body’s adequate blood supply.
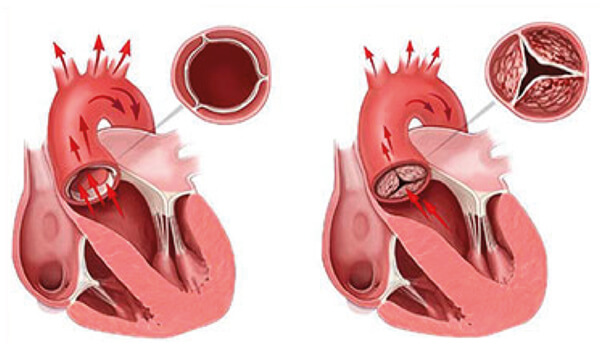
Schematic representation of a normal aortic valve (left) and a calcified valve (right), showing significant restriction in opening and a reduced volume of blood ejected from the heart into the systemic circulation.
The main symptoms experienced by patients include shortness of breath, easy fatigue, chest pain, dizziness, and fainting episodes. Once symptoms appear, the mortality rate is very high—estimated at about 25% within the first year and 50% within two years. There is no medication that can adequately treat this condition. The only effective therapy is aortic valve replacement, which can be performed either surgically or percutaneously using catheter-based techniques.
Surgical Aortic Valve Replacement (SAVR) has been the standard treatment for this condition for many years. The procedure is performed under general anesthesia and requires opening the patient’s chest and temporarily stopping the heart. The surgeon removes the calcified valve and implants a new mechanical or bioprosthetic valve. The operation typically lasts about four to five hours. Patients usually remain in the hospital for about a week and can generally return to their normal activities within two months.
Aortic valve stenosis predominantly affects elderly individuals. In this patient group, the coexistence of other medical conditions is very common—such as coronary artery disease, stroke, renal failure, respiratory failure, liver failure, peripheral vascular disease, pulmonary hypertension, malignancies, and nutritional disorders. These factors significantly increase the risk of surgical intervention, leading both physicians and patients to seek alternatives whenever possible. It is estimated that around 33% of patients over 75 years of age with severe aortic stenosis are not offered surgical treatment because of the high procedural risk.
Transcatheter Aortic Valve Replacement (TAVR or TAVI) is a recently developed technique that allows the implantation of a new bioprosthetic valve in place of the diseased, degenerated one—without the need for open-heart surgery involving chest opening and temporary interruption of the heart’s function. The procedure typically lasts about two hours. Patients usually remain in the hospital for four to six days and are able to fully resume their activities within one week. The number of patients undergoing transcatheter aortic valve implantation has increased dramatically over the past decade, approaching 200,000 worldwide.
Patient Selection for TAVR
Transcatheter aortic valve replacement (TAVR) is currently offered only to patients for whom surgical valve replacement is contraindicated or considered to carry a very high risk of complications. Candidate patients undergo a series of examinations to determine whether they are suitable for this therapeutic approach. These evaluations may be performed either during a hospital admission or on an outpatient basis. The assessment typically includes:
- Comprehensive hematological and biochemical testing: measurement of hematocrit and platelets, evaluation of renal and liver function
- Echocardiogram: assessment of overall cardiac function and valve performance.
- CT angiography of the thoracic and abdominal aorta and iliofemoral arteries: visualization of vessel size, course of major arteries, and morphology of the aortic valve.
- Coronary angiography and right heart catheterization: detection of coronary artery stenosis and measurement of intracardiac and pulmonary pressures.
- Spirometry and pulmonary function tests: evaluation of respiratory function.
- Carotid triplex ultrasound: detection of carotid artery stenosis.
- Anesthesiology consultation: determination of the safest anesthesia approach and evaluation of potential risks.
- Cardiac surgery consultation: assessment of the risks of conventional surgical valve replacement and alternative therapeutic options.
- Interventional radiology consultation: evaluation of cardiac function, detailed explanation of the TAVR procedure, and discussion of potential complications.
The results of all examinations are collected and carefully evaluated. A risk index (EUROSCORE or STS SCORE) is calculated to estimate the potential risk of conventional surgical aortic valve replacement. A specialized Heart Team, consisting of an interventional cardiologist, a cardiac surgeon, and physicians from other specialties, collectively decides whether the patient is an appropriate candidate for transcatheter aortic valve replacement (TAVR). The patient is then fully informed, and if deemed suitable, returns to the hospital at a later date to undergo the procedure.
Indications for Transcatheter Aortic Valve Replacement include patients:
- with STS SCORE > 10 or EUROSCORE > 20
- of advanced age
- who are considered “frail” with severe nutritional disorders
- with severe calcification of the ascending aorta (porcelain aorta)
- who have undergone previous cardiac surgery
- with a history of chest radiotherapy
- with severe comorbidities
- with advanced respiratory failure
- with liver cirrhosis and portal hypertension
- with thoracic deformities making open-heart surgery impossible
- with severe degenerative neuromuscular diseases
Technique
The procedure is performed in the Cardiac Catheterization Laboratory by a team of specially trained interventional cardiologists and cardiac surgeons, known as the Heart Team. The team also includes anesthesiologists, vascular surgeons, nurses, and medical technology specialists. The process is similar to that of coronary angiography or angioplasty. An expandable bioprosthetic valve is mounted on a catheter, advanced through the patient’s arteries to the site of the narrowed aortic valve, and deployed in place either by balloon inflation or by a dedicated release mechanism. The new valve pushes the diseased one against the walls of the aortic root and begins functioning immediately. The success rate of valve implantation by experienced interventional cardiologists exceeds 98%.
The most common access route for the catheter is through the femoral artery. In patients with severe narrowing of the leg arteries, alternative access sites are used. The most frequently employed approaches are:
- Transfemoral access: The catheter with the prosthetic valve is advanced through the femoral artery.
- Transapical access: A small incision is made in the chest, and the catheter is advanced through the apex of the heart.
- Transaortic access: A small incision is made in the chest, and the catheter is advanced through the ascending aorta.
- Transsubclavian access: The catheter is advanced through the subclavian artery.
Worldwide, the most commonly used transcatheter aortic valves are the Medtronic CoreValve and the Edwards SAPIEN. Each valve has distinct characteristics, advantages, and disadvantages. The choice of valve is made on an individualized basis for each patient.

The most commonly used prosthetic aortic valves in transcatheter aortic valve replacement (TAVR) are: Α: Medtronic CoreValve® Β: Edwards SAPIEN®.
Medtronic CoreValve®:
This bioprosthetic valve is made from porcine pericardial tissue mounted on a nitinol frame. It is available in four sizes. The valve is self-expanding and is deployed in the correct position using a specially controlled release mechanism.
Medtronic CoreValve® – Controlled Release Mechanism.
Edwards SAPIEN® Valve:
This bioprosthetic valve is made from bovine pericardial tissue mounted on a cobalt-chromium frame. It is available in three sizes. The valve is deployed at the intended site by balloon expansion, which ensures precise positioning and immediate function once fully expanded.
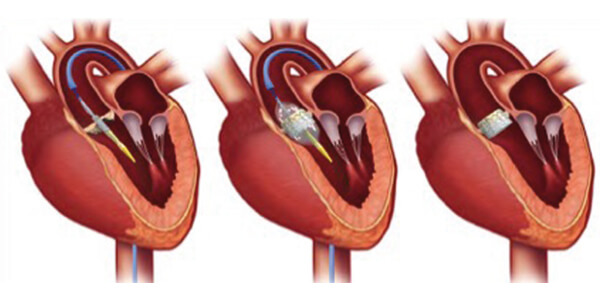
Edwards SAPIEN® Valve – Balloon Expansion Deployment.
Complications
As with any medical procedure, transcatheter aortic valve replacement (TAVR/TAVI) may be associated with complications. The likelihood of severe complications is low, estimated at less than 2%. In any case, the risk is lower than that of conventional surgical aortic valve replacement. The most common complications include:
- Stroke
- Bleeding or vascular complications at the access site
- Need for permanent pacemaker implantation
- Myocardial infarction
- Kidney function disorders
- Prosthetic valve insufficiency
- Displacement of the prosthetic valve requiring urgent cardiac surgery
- Prosthetic valve infection
- Death
Hospitalization, Medication, and Follow-up
The patient is typically hospitalized for one to two days in the Cardiology Intensive Care Unit, followed by an additional two to three days in a regular ward. Mobilization usually occurs on the second or third day.
Medication involves a combination of antiplatelet and/or anticoagulant agents. After the first six months, the regimen is further simplified.
The physician reassesses the patient within the first month following the transcatheter procedure and determines the schedule for subsequent follow-up visits.
Improvement in cardiac symptoms is usually immediate, and after hospital discharge, the patient can quickly return to daily activities. It should be emphasized that after the first month, the presence of the prosthetic valve is not a contraindication for undergoing magnetic resonance imaging (MRI).
Summary
Transcatheter Aortic Valve Replacement (TAVR) represents a novel and highly effective therapeutic option for selected patients with severe aortic valve stenosis for whom conventional surgical treatment is either contraindicated or carries a very high risk. The procedure offers an extremely high success rate while maintaining a very low incidence of complications. TAVR significantly reduces patient discomfort, shortens hospital stay, and markedly improves quality of life.
It is highly likely that in the near future, with technological advancements and reduced costs, transcatheter replacement will largely supplant surgical aortic valve replacement.
Georgios Karavolias
Interventional Cardiologist, Cardiology Clinic Director, Metropolitan Hospital
Hemodynamics Laboratory – Interventional Cardiology

The Hemodynamics Laboratory of Metropolitan Hospital is one of the few centers in Greece with special certification from the Ministry of Health and the Central Health Council for performing: Transcatheter Aortic Valve Implantation (TAVI/TAVR) and Transcatheter Mitral Valve Repair using the MitraClip system.