As soon as you visit the Metropolitan Hospital Radiation Oncology Center, you will be approached by a dedicated team of specialists, who will tailor the treatment to your individual needs. Apart from radiation oncologists, this specialized team includes the Medical Physics Department, staffed by radiophysicists trained in the latest radiotherapy technologies, radiotherapy technicians, nursing staff and administrative staff. Our team also works closely with all the medical specialists involved in central nervous system tumors, such as neurosurgeons, neurologists, medical oncologists, neuroradiologists and anatomic pathologists. This guarantees the most individualized, modern and effective treatment, with the least possible side-effects. This impeccable collaboration is further forged through the Hospital’s weekly Oncology Council meetings, with staff from all the relevant medical specialists participating.
The state-of-the-art radiotherapy techniques and the skills acquired by the doctors from their training in centers of excellence in Europe and the USA ensure highly accurate and targeted tumor treatment, by delivering the maximum radiation dose possible, with the least damage to healthy cells.

Three-dimensional Conformal Radiotherapy
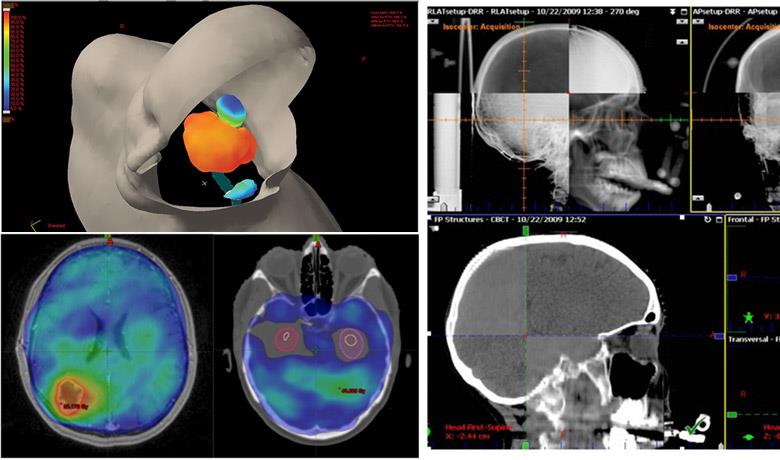
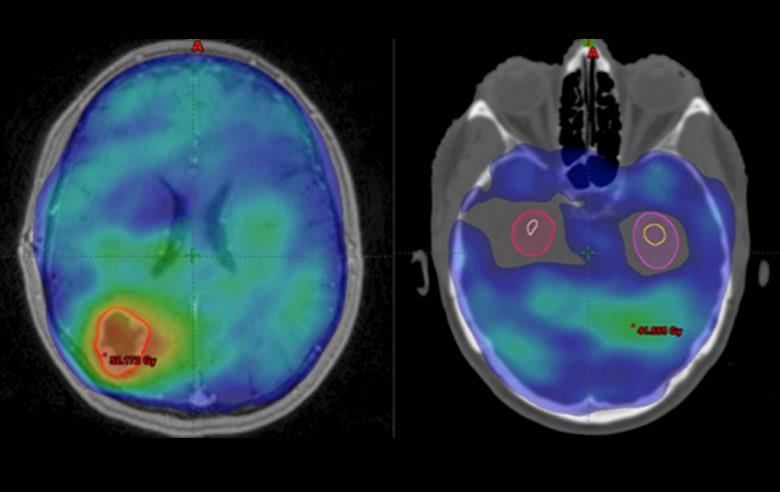
Three-Dimensional Conformal Radiotherapy (3D-CRT) is a technique that uses 3D CT images to design the treatment plan. As a result, the radiation fields are based on the exact shape of the targeted tumor. This increases accuracy when targeting the tumor and reduces the dose to the surrounding healthy tissue, compared to the older 2D radiotherapy techniques.
In addition, it offers us the opportunity to find out the exact dose received by each part of the tumor and the normal tissue, through the study of special diagrams known as Dose Volume Histograms (DVH). This allows us to select the appropriate treatment plan offering the best coverage of the target volume, minimizing the radiation dose to normal organs. Specifically, we must make sure that the selected plan is associated with less than 10% mild side-effects and less than 0.5% severe side-effects.
Intensity Modulated Radiotherapy (IMRT)
Intensity Modulated Radiotherapy (IMRT) is an advanced type of highly accurate and targeted radiation therapy that is considered the next generation in 3D-CRT, used by most radiotherapy centers in Greece.
As evident in Image 4, IMRT further improves the possibility of adjusting the high radiation doses to the shape of the tumor, reducing the burden received by normal tissue.
IMRT allows radiation oncologists to deliver adequate doses to tumors located very close to critical central nervous system structures, such as the optic nerves, the optic chiasm, the trunk, etc. Without IMRT, these tumors would not have been able to receive the necessary radiation dose, compromising the patient’s recovery chances.
In addition, IMRT, and especially its most contemporary form, Volumetric Modulated Arc Therapy (VMAT), achieves must greater dose distribution in demanding treatment plans, such as radiation therapy to the axon, while reducing the side-effects (e.g. memory disorders) in patients with brain metastases, protecting the area of the hippocampus. It is also possible to deliver greater radiation doses to brain metastases that are visible in imaging scans (greater chance of controlling the disease) and lower prophylactic doses to the rest of the brain (fewer side-effects). In our Center, we use the latest technology by Varian, the RapidArc IMRT.
Image Guided Radiotherapy
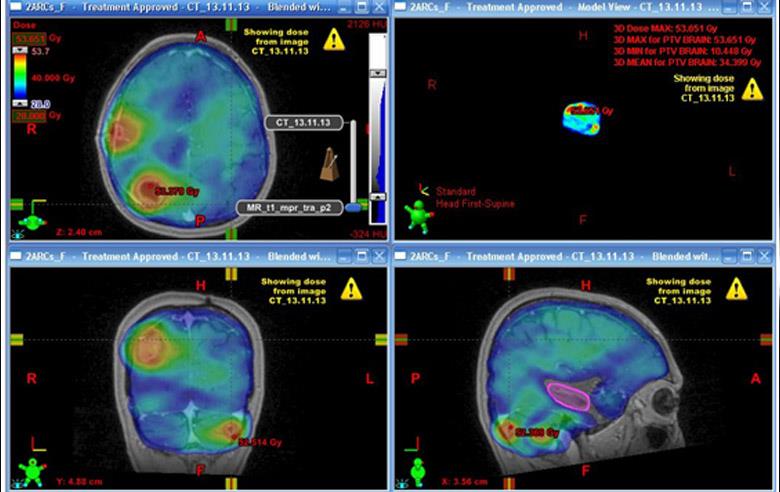
Image Guided Radiotherapy (IGRT) is a technique that performs an image scan of the patient in the treatment position, prior to every radiotherapy session. Imaging is 2D (ExacTrack, Brainlab®, Image 7) or 3D (Cone Beam CT, Image 8). This greatly increases the accuracy of the radiotherapy and reduces the risk of error upon placement of the patient.
IGRT makes radiotherapy more accurate, while lowering the chance of underdosing the tumor or overdosing the normal tissue. It also makes it possible to reduce the necessary margins placed around the tumor to counteract the uncertainties of treatment. As a result, we may decrease the size of the radiation field and consequently irradiate smaller areas of normal tissue, with fewer side-effects for the patients.
Lastly, the great accuracy and the smaller safety margins allow us to deliver large radiation doses daily if necessary, without increasing the risk of toxicity. Large daily doses are delivered by many modern radiotherapy techniques, such as Stereotactic Radiosurgery (SRS).
Stereotactic Radiosurgery
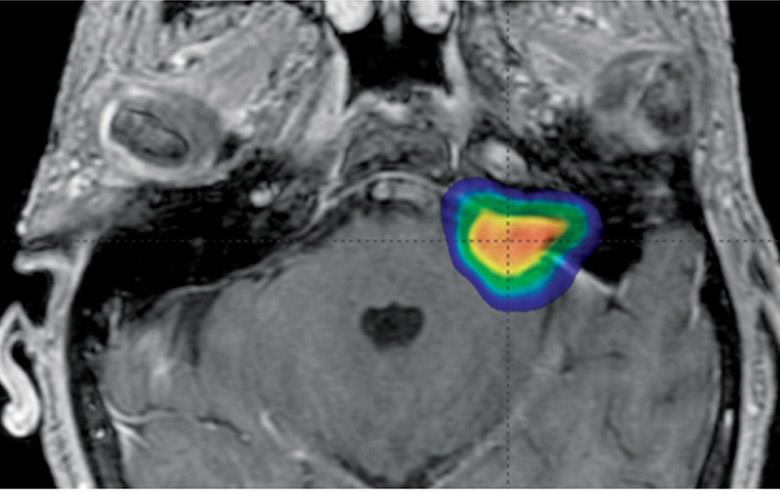
Stereotactic Radiosurgery (SRS) is a non-invasive radiotherapy technique that targets brain tumors and functional abnormalities.
SRS has 3 main traits:
- Very high accuracy (1-2 mm).
- Very high conformity, with sharp dose decrease on the border of the targeted tumor, leading to the least possible irradiation of the surrounding normal tissue.
- Delivery of a very large radiation dose daily. The radiation therapy is concluded in 1 to 5 sessions; however, it is possible to have more sessions performed, e.g. for large tumors or in cases of re-irradiation (Fractionated Stereotactic Radiotherapy - FSRΤ).
SRS is an excellent alternative to interventional surgery, especially when patients cannot undergo surgery or in cases of inoperable tumors and intracranial abnormalities.
SRS is indicated for:
1. Benign and malignant brain tumors:
- Primary malignant brain tumors (< 4 cm) - for delivery of booster dose or for rescue treatment in the event of recurrence (astrocytoma, glioma, glioblastoma multiforme, oligodendroglioma)
- Brain metastases
- Acoustic neuroma
- Meningioma
- Pituitary adenoma (recurrence or residual disease)
- Eye tumors
- Skull base tumors
- Hemangiomas
- Craniopharyngiomas
2. Vascular disorders:
- Arteriovenous malformations
3. Functional abnormalities:
- Trigeminal neuralgia
- Epilepsy
- Parkinson’s disease
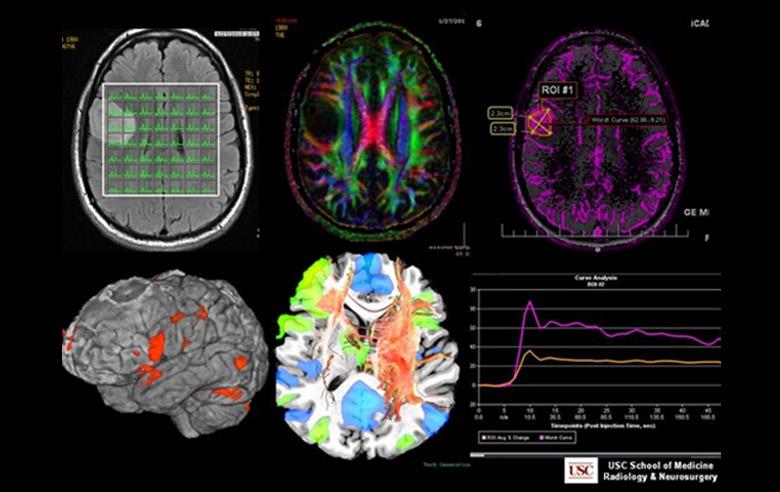
MRI Spectroscopy & Perfusion
Fusion of CT images with MRI, MRI Spectroscopy and Perfusion images: This way, radiation oncologists may trace the tumor, as well as all the normal organs visible in the MRI (such as the optic chiasm, the optic tract, the trunk, etc.), with greater accuracy. In addition, MRI Spectroscopy makes it easier to detect recurrences in areas of the brain that have been irradiated or operated on. Lastly, digital and/or magnetic angiography is necessary for tracing vascular disorders of the central nervous system, such as arteriovenous malformations (AVM).