The path toward aging naturally brings changes in memory and cognitive function. Forgetfulness is relatively normal as people grow older. What is not normal, however, is memory loss to the extent that it affects a person’s independence or personal safety. Such memory problems are often accompanied by changes in mood, personality, or behavior.
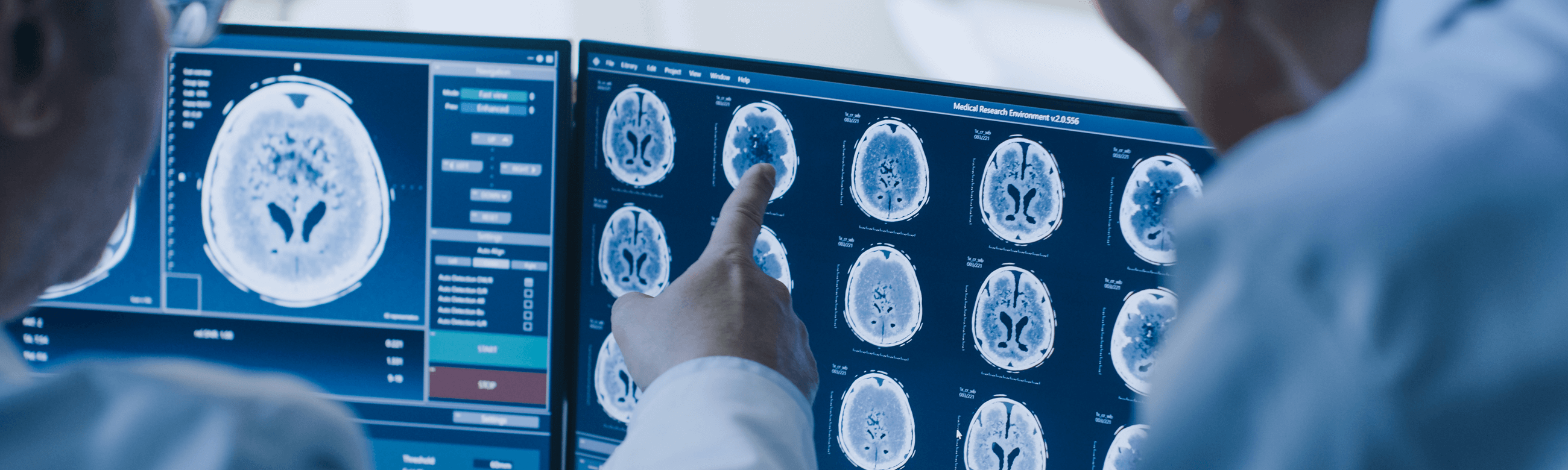
Brain & Behavior: Neuropsychology Department
Neuropsychology examines the relationship between the brain and behavior. In clinical practice, the neuropsychologist assesses how the brain is functioning at a given time by evaluating both cognitive abilities and the emotional/psychological state of the individual through specialized neuropsychological tests.
A key principle of neuropsychological assessment is determining whether an individual functions at their premorbid optimal level or whether there is deterioration in a specific cognitive or psychological domain.
This question is crucial in clinical practice, as it directly relates to the diagnosis and treatment of a wide range of conditions, including:
- Alzheimer’s disease and related dementias
- Parkinson’s disease
- Neurodegenerative disorders
- Epilepsy
- Traumatic brain injury
- Brain tumors
- Psychiatric conditions
Metropolitan Hospital Memory Clinic
The Memory Clinic at Metropolitan Hospital specializes in caring for patients with memory problems, potential cognitive decline, or behavioral and personality changes, as well as supporting their relatives and caregivers.
Developed in collaboration with the Neurology Department, the clinic integrates neurological expertise, clinical neuropsychology, and advanced diagnostic technologies to provide accurate diagnosis and effective management of dementia.
Neuropsychological Assessment at the Memory Clinic
Alzheimer’s disease and dementias affect higher cognitive functions. The only valid way to diagnose them is through clinical neuropsychology and the mapping of a neuropsychological profile. This involves structured questioning and cognitive testing to evaluate brain function. Neuropsychological assessment is officially recognized as a clinical procedure for evaluating memory disorders, particularly when diagnosis is unclear. Its results are essential for both diagnosis and treatment planning, in collaboration with the neurologist and, when necessary, a multidisciplinary team (radiologist, internist, psychiatrist, clinical psychologist).
At present, clinical neuropsychology—together with medical history—remains the most scientifically reliable method for detecting even subtle cognitive changes, often before they appear on brain imaging (MRI, CT).
At Metropolitan’s Memory Clinic, assessments are performed with specialized, sensitive tests that have been extensively validated in both research and clinical populations, and standardized by gender, age, and education level.
Memory Evaluation with CANTAB Mobile
CANTAB Mobile is a scientifically validated tool for the early detection of memory disorders. Its primary goal is to identify the first signs of clinically significant memory decline, enabling timely intervention.
Delivered via iPad, it combines a sensitive memory test—used in Alzheimer’s research for over 30 years—with a mood assessment to differentiate depression from cognitive decline. It has been successfully incorporated into the UK’s national Alzheimer’s strategy. In 2013, Cambridge Cognition, the developer of CANTAB, received special recognition from UK Prime Minister David Cameron at the G8 Dementia Summit.
At Metropolitan’s Memory Clinic, CANTAB Mobile testing is now a standard component of neuropsychological evaluation for memory disorders.
- Cormack F., Barnett JH., Nidos A. Characterising Profiles of Impairment in AD, MCI and SMI Using a Brief Computerised Battery. Alzheimer's Association International Conference (AAIC) 2015. July 18 - 23, 2015; Washington, DC.
- Nidos A., Kasselimis D., Zavitz K., Cormack F. Diagnostic value of a cognitive battery for assessing cognitive decline. To be presented at the 10th Clinical Trials on Alzheimer's Disease (CTAD) November 1-4, 2017; Boston, USA.
What causes memory disorders?
Abnormal memory loss may stem from reversible conditions such as depression, stress, substance or alcohol abuse, infections, or poor nutrition. It may also appear as a symptom of other medical conditions. Early and accurate diagnosis, combined with treatment, can significantly improve these situations. Extensive memory loss, however, is often associated with neurodegenerative diseases, including:
- Mild Cognitive Impairment (MCI)
- Alzheimer’s disease and related dementias
- Vascular dementia
- Parkinson’s disease
- Traumatic brain injuries
In some cases, the first symptom may be an abnormal personality change.
With accurate diagnosis and appropriate treatment planning, patients with Alzheimer’s and other dementias can maintain their highest possible level of independence and improve their quality of life.
Memory Clinic Services
- Neurological examination
- Neuropsychological assessment
- Laboratory testing
- Neuroimaging (MRI, CT scans)
- Treatment planning and intervention
- Counseling for caregivers and family members
The Memory Clinic team includes a neurologist and a clinical neuropsychologist, with additional support from neuro-radiology and internal medicine specialists as needed. The goal is early and accurate diagnosis of memory problems and the development of a personalized treatment plan.
What to expect at the Memory Clinic
During the first visit, lasting 1–2 hours, patients undergo an initial assessment of memory and cognitive function to determine the severity of the issue and its underlying cause.
If required, patients proceed to laboratory and diagnostic testing (blood tests, EEG, MRI, CT).
Neuropsychological Assessment
In a subsequent stage, the clinical neuropsychologist conducts standardized neuropsychological testing focusing on memory, attention, perception, and problem-solving. The evaluation results in a detailed cognitive profile that highlights deficits and clarifies the link between brain and behavior.
Treatment Planning
Intervention is personalized and may include: medication, psychotherapy, management of dementia-related behavioural symptoms, cognitive rehabilitation and exercises. Throughout the process, the team works closely with caregivers and family, providing counseling and psychological support.
“Modern neuroscience has mapped the brain regions responsible for memory. Today’s clinical and research advances help us understand the causes of memory disorders and the ways to address them.”
The clinic was designed and implemented by the scientific team of the Neurology Department at Metropolitan Hospital, with the goal of combining outstanding neurological clinical practice, clinical neuropsychology, and the latest technological and diagnostic methods for the diagnosis and management of dementia.
Memory Clinic Goals
- Early diagnosis: Mild Cognitive Impairment – Dementia – Alzheimer’s
- Treatment planning
- Cognitive rehabilitation and strengthening
- Family and caregiver counseling