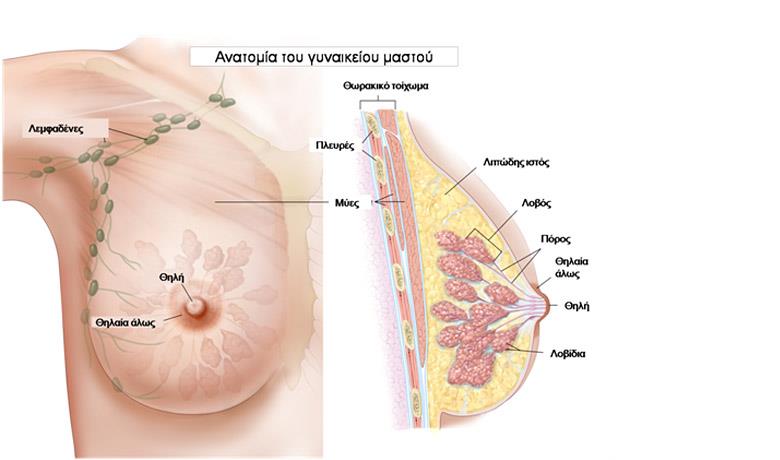
The external anatomy of the breast consists of the nipple and the areola. The nipple consists of a red to brown projection in the breast skin, located slightly below and away from the center of the breast. The tip of the nipple has openings for about 15-20 lactiferous ducts (milk ducts). The areola is a small circular and slightly protruding area around the nipple. Internally, the breast consists of glandular and adipose tissue. The mammary gland is located behind the areola and consists of milk producing lobules and lactiferous ducts that transfer the milk through the lactiferous sinus to the nipple. Lymphatic drainage of the breast is achieved via the axillary and then the subclavicular lymph nodes.

BREAST CANCER DEVELOPMENT
Breast cancer can start off from the cells of the milk ducts (ductal carcinoma) or the lobules (lobular carcinoma). These cells undergo gene mutation resulting in cellular multiplication at an extremely fast rate. In the early stages, precancerous lesions (non-invasive ductal or lobular breast cancer) may appear as calcifications in a mammogram.
However, with time, these lesions may turn into cancer. They then acquire the ability of making new vessels to feed the tumor. The tumor grows and at some point in its development, its cancer cells may acquire the ability to escape from the primary site and either migrate to lymph nodes or to the body’s other organs (metastasis).
EPIDEMIOLOGICAL DATA

Breast cancer is one of the most common forms of cancer in the world and ranks first among the female population. In Greece, 4,500 new cases are reported each year, while it is estimated that on a global scale 1 in 8 women will develop breast cancer at some point in their life. In Europe, 60% of breast cancer cases are diagnosed at the early stage. Male breast cancer is rare with about 100 times less frequency compared to women and with the same survival rates.
However, breast cancer mortality rates are declining, which is attributed to early diagnosis via mammograms and improved treatments.
ETIOLOGICAL FACTORS
Below are factors which have been more or less correlated with an increased likelihood of developing breast cancer.
- Inheritance: It is estimated that just 5-10% of breast cancer incidence is actually related to hereditary factors. Nevertheless, 8 in 10 women who have a BRCA 1 or BRCA 2 gene mutation will develop breast cancer (and/or ovarian cancer). In addition, women who have blood relatives with breast cancer (especially at a young age) have a higher risk of developing breast cancer.
- Age: Breast cancer rates increase with age. Most cases occur among women aged 50+ years, while it is rare for women to develop breast cancer under 35 years (5% of cases), with the exception of those that have a genetic predisposition.
- Menstrual disorders: Women who started menstruating early in life or go through menopause later in life have a higher risk of developing breast cancer.
- History of cancer: Women who have previously developed ovarian or breast cancer have a higher risk of developing a 2nd breast cancer.
- Childless women.
- Hormone Replacement Therapy: It provides relief from menopause symptoms; however, its long-term use after menopause increases the risk of developing breast cancer.
- Smoking: It appears that smoking is associated with the relative risk of developing breast cancer.
SYMPTOMS AND DIAGNOSIS

The main breast cancer symptoms include:
- Lump or hardening of the breast areas and/or the axilla
- Swollen lymph nodes, such as the axillary
- Discharge or blood from the nipple
- Skin inversion, namely nipples that suddenly start to point inward toward the breast
- Redness, sensitivity or chest pain
Early stage breast cancer does not have symptoms. A palpable mass, change in skin color, inversion or discharge appears at a later stage. If a women disregards these symptoms, then she may develop signs of advanced disease, such as a breast that is warm to the touch and red (inflammatory cancer), bone pain and extensive swelling.
Diagnosis of early or precancerous breast cancer (non-invasive breast cancer) is on the rise due to women’s awareness in terms of their breast check-up with a clinical breast examination, mammogram and ultrasound, as well as self-examination. As soon as a suspicious tumor is detected, diagnosis is possible by obtaining tissue from the tumor for microscopic examination. There are 4 diagnostic methods:
- Cytology examination: This is done using a fine needle (FNA - Fine Needle Aspiration), which is adapted to a syringe and allows the aspiration of cells from the suspicious site of the breast.
- Histological biopsy: In this case the needle is bigger, local anesthesia and an incision are required and part of the tissue is examined.
- Stereotactic biopsy: Histological material is collected under guided stereotactic imaging.
- Open surgical biopsy: The lesion is identified using rapid biopsy during surgery, prior to removing the tumor.
PROGNOSTIC FACTORS

As with all types of cancer, disease prognosis is associated with the size of the tumor, lymph node metastasis or not (as well as the number of infiltrated lymph nodes) and remote metastasis or not. Moreover, in the case of breast cancer, the biological properties and molecular characteristics of the tumor play a significant role. These include the presence of hormonal receptors, the cell proliferation marker, genetic mutation, etc.
In conjunction with the patient’s age, these tumor characteristics not only determine disease prognosis, but also the therapy that needs to be followed after surgery.
TREATMENT / RADIATION THERAPY
Breast cancer treatment may include surgical excision, radiation therapy and chemotherapy, or a combination of these treatments.

Radiation Therapy
A high-energy X-ray beam targets the affected area using a special machine known as a linear accelerator. Radiation therapy is a local treatment that is delivered to the breast after lumpectomy or the thoracic wall after mastectomy. On occasion it may include subclavian or axillary lymph nodes.
Radiation therapy is always indicated in the treatment of invasive breast cancer (and in most non-invasive breast cancers) after lumpectomy where the affected breast has not been removed. Specifically, the use of radiation therapy made conventional breast surgery possible, giving the same success rates as those of mastectomy [1]. In the event that the tumor has been removed with a mastectomy, radiation therapy has specific indications that are associated with the existence of infiltrated axillary lymph nodes, tumor size, etc., and in these cases it appears to increase local control of the disease and overall survival.
Three Dimensional Conformal Radiotherapy (3D-CRT) is the most frequently used external beam radiation therapy technique, while Intensity Modulated Radiotherapy (IMRT), an improved version of 3D-CRT which focuses the dose on the target and avoids healthy tissues, has been increasingly gaining ground over recent years. The application of IMRT made using state-of-the-art and more precise image guided radiotherapy (IGRT) of the targeted area prior to the radiation therapy all the more necessary.
It is important for the treatment decision to be taken after the patient is informed about treatment options and any associated complications or toxicities. For example, a woman with a tumor in her left breast would benefit more from IMRT, which would protect her heart (which is located opposite the left breast) from radiation and would reduce the risk of coronary disease in the future. Nevertheless, well-studied side effects include dermatitis and fibrosis in the irradiated breast, whereby IMRT has demonstrated the best aesthetic results compared to traditional radiation therapy.
SIDE EFFECTS FROM RADIATION THERAPY

Skin reaction: During radiation therapy, the skin and hair in the irradiated area will undergo changes. It is normal and to be expected. After 2-3 weeks, your skin color will change resembling a sun tan. As treatment goes on, it may turn bright red or very dark. You may also feel that your skin is dry, peels easily and itches. Sometimes the nipple area becomes slightly tender. Dermatitis will gradually subside; usually 3-4 weeks after radiation therapy is completed.
Breast discomfort and swelling: Most women experience breast tenderness, especially in the nipple area, when skin changes start. In addition, some experience a certain degree of breast swelling. In this case, you may feel pinching and that your breast is heavy and swollen. If you have undergone axillary lymph node removal, it is possible that you will experience some stiffness in the corresponding shoulder following surgery. In this case, stiffness may worsen with radiation therapy, especially if the axillary and subclavian areas are being irradiated.
Fatigue: Some women experience fatigue 2-3 weeks after treatment. Fatigue is usually described as tiredness, lethargy, weakness, and difficulty concentrating. These symptoms gradually pass after treatment is completed.
OUR APPROACH

At Metropolitan Hospital we offer state-of-the-art radiation therapy techniques to treat breast cancer. These include:
- More conformal dose distribution, resulting in the protection of the heart in left breast irradiation
- More uniform dose distribution, resulting in less dermatitis and a better aesthetic result
- Simultaneous tumor bed boost, resulting in treatment reduction by 1-2 weeks
- Simultaneous bilateral breast cancer irradiation when breasts cancer occurs in both breasts simultaneously
The state-of-the-art radiotherapy techniques and the skills acquired by the doctors from their training in centers of excellence in Europe and the USA ensure highly accurate and targeted tumor treatment, by delivering the maximum radiation dose possible, with the least damage to healthy cells. Compared to conventional radiation therapy, APBI has the following advantages:
- APBI is performed at the same time or a few weeks after tumor removal and the catheters remain in place for 4-5 days.
- APBI is delivered twice a day for a period of 4-5 days, while conventional radiation therapy usually lasts 6 weeks.
- Radiation therapy treatments are focused on tissues that surround the tumor cavity, avoiding healthy tissue and organs close to the breasts, such as the heart and lungs.