The lungs are two organs that resemble sponges and are located inside the thoracic cavity. The right lung is divided into 3 sections known as lobes, while the left lung has 2 lobes. When you inhale, air passes through the mouth and reaches the lungs via the trachea (windpipe). The trachea is divided into tubes known as bronchi, which then branch out into smaller and smaller tubes called bronchioles, eventually leading to air sacs called alveoli.
A lot of tiny blood vessels known as capillaries surround the alveoli, absorbing the oxygen from the inhaled air in the alveoli and diffusing the carbon dioxide that has been formed in the body. The latter is exhaled into the air.
Situated between the two lungs is the mediastinum, which contains the heart, the esophagus and the great vessels. Also found in the mediastinum are the lymph nodes that drain lymphatic fluid from the lungs.
LUNG CANCER DEVELOPMENT
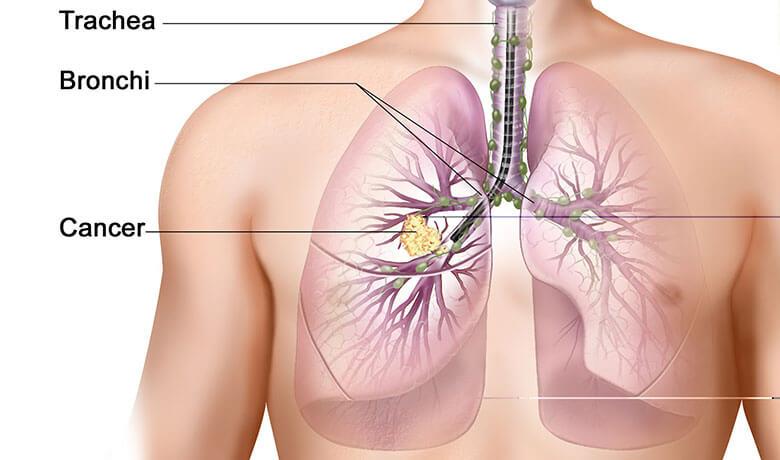
It is possible for lung cancer to originate in the bronchial, bronchiolar and alveolar cells. These cells undergo gene mutation (e.g. under the influence of substances contained in smoke), resulting in cellular multiplication at an extremely fast rate. In the beginning, sites with precancerous lesions appear, which do not cause symptoms and are not visible on X-ray.
However, with time, these lesions may turn into cancer. They then acquire the ability to create new vessels that feed the tumor, which grows enough to be seen in imaging, such as X-ray and chest CT.
At some point during disease development, the cancer cells may acquire the ability to escape from the primary site and either migrate to lymph nodes or to the body’s other organs (metastasis).
EPIDEMIOLOGICAL DATA
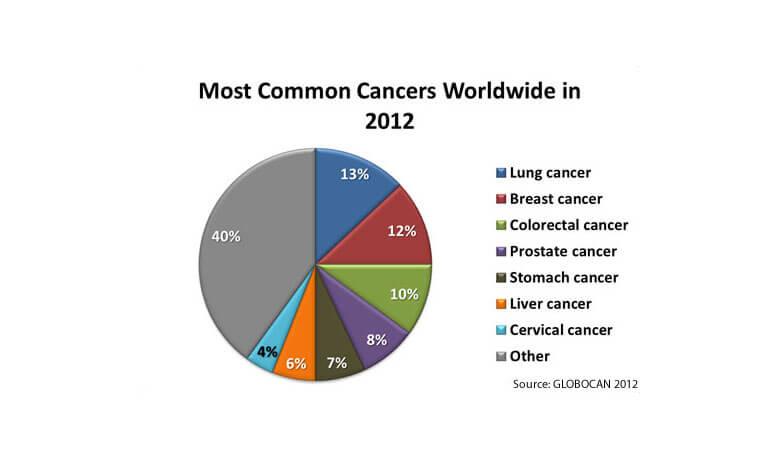
Lung cancer is the second most common cancer in both men and women. The average age at the time of diagnosis is about 71.
Overall, the chance that an individual will develop lung cancer in their lifetime is about 1 in 15. For smokers the risk is much higher, while for non-smokers the risk is lower.
The lung cancer rate has been dropping among men over the past few decades, but the corresponding rates among women have only recently started dropping, after a long upward trend.
ETIOLOGICAL FACTORS

Smoking or exposure to smoke in any form is the most significant risk factor for lung cancer. Non-smokers that inhale secondhand smoke (passive smokers) are also at a high risk of developing the disease.
A smoker can reduce the risk of developing lung cancer by quitting. If someone has been diagnosed with lung cancer and undergoes cancer treatment, research has shown that quitting smoking may increase the efficiency of the treatment.
Although smoking is the most significant risk factor, one in five lung cancer patients has never smoked. Other risk factors include exposure to asbestos and radon, while in some patients there is no known lung cancer cause.
SYMPTOMS AND DIAGNOSIS
The main lung cancer symptoms include:
- Persistent cough or change in existing chronic cough
- Lung infection that does not go away or relapses
- Blood in saliva
- Hoarseness in the voice that does not go away
- Shortness of breath and wheezing
- Chest pain while coughing or breathing deeply
- Loss of appetite and weight
- Difficulty swallowing
- Fatigue and sleepiness
Diagnosis is usually made in the context of investigating some of these symptoms. An X-ray is the first screening test performed which may show the lung cancer. This is followed by a chest CT, to show the precise location of the tumor and to assess the mediastinal lymph nodes. A biopsy of the cancer and/or any suspicious lymph nodes is then necessary because the histological type of the tumor and the extent of the disease will determine the type of treatment. The biopsy is performed via bronchoscopy and when this is not feasible, it can be performed via CT-guided percutaneous needle biopsy. Finally, in some cases the tumor can be identified via a cytology examination of the patient’s sputum.
Other diagnostic tests that can be performed include:
- CT of the abdomen and brain
- Bone scintigraphy
- PET–CT
- Endoscopic ultrasound (EUS)
TYPES OF LUNG CANCER

Lung cancers are classified into two types
1. Non-small cell lung cancer (NSCLC): Accounts for about 85% to 90% of all cases and is divided into 3 sub-types, based upon the microscopic appearance of the tumor cells. They belong to the same group, though, because their treatment and prognosis is similar. They are:
- Adenocarcinoma: It accounts for about 40% of cases and while it is associated with smokers, this is the most common type of lung cancer seen in non-smokers. It is most common in young women.
- Squamous cell carcinoma: It accounts for about 30% of cases and is associated with smoking. It is most frequently located in the central chest area, close to the bronchi.
- Large cell carcinoma: It accounts for about 15% of cases. A subgroup known as large-cell neuroendocrine carcinoma closely resembles small cell lung cancer.
2. Small cell lung cancer (SCLC): It accounts for about 15% of cases and is named as such because of the small size of its cells under the microscope. It rarely appears in non-smokers. It usually metastasizes rapidly to many sites within the body. Nonetheless, it usually responds quickly to chemotherapy and radiation therapy.
TREATMENT / RADIATION THERAPY

Treatment
Lung cancer treatment includes surgical excision, radiation therapy and chemotherapy, or a combination of these treatments.
Radiation Therapy
In the case of early stage non-small cell lung cancer, surgical excision of the tumor is usually the first treatment choice. If health reasons prevent the patient from undergoing surgery, then radiation therapy, and in particular a technique known as extracranial stereotactic radiotherapy, can offer significant results, yielding a local control rate in up to 90% of cases [1].
For larger, more aggressive tumors (NSCLC) that are inoperable, primary treatment consists of radiation therapy frequently in conjunction with chemotherapy. Chemotherapy is usually administered at the same time as radiation therapy, but in some cases it may be administered before. Radiation therapy is also indicated after surgery when the tumor has not been completely removed, or when it relapses.
In the case of small cell lung cancer, radiation therapy is indicated after chemotherapy has been completed, primarily in limited disease, while prophylactic cerebral irradiation is performed on most patients.
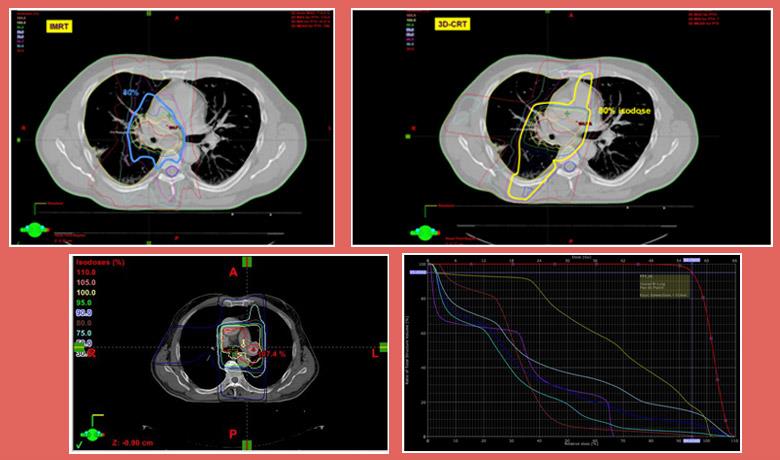
External beam radiation therapy uses high-energy X-rays (photons) to treat lung cancer. The rays are produced by a linear accelerator, positioned at a distance from the patient’s body. Three Dimensional Conformal Radiotherapy (3D–CRT) is the most frequently used external beam radiation therapy technique, while Intensity Modulated Radiotherapy (IMRT), an improved version of 3D-CRT which focuses the dose on the target and avoids healthy tissues, has been increasingly gaining ground over recent years.
The application of IMRT made using state-of-the-art and more precise image guided radiotherapy (IGRT) of the targeted area prior to the radiation therapy all the more necessary. Moreover, with respect to lung cancer, respiration-induced tumor motion makes using techniques based on which we can determine the extent of motion and adapt the radiation therapy treatment plan (4D0CT) all the more necessary.
It is important for the treatment decision to be taken after the patient is informed about treatment options and any associated complications or toxicities.
Contemporary radiation therapy techniques have managed to reduce lung cancer treatment side effects. Focusing on high-dose radiation on a tumor, with less impact on healthy organs, thanks to IMRT and stereotactic radiotherapy, but also the safety that these doses will be precisely delivered to the target, thanks to IGRT and 4D-CT, have established radiation therapy as extremely safe in lung cancer treatment. Thus, we are now able to deliver high doses of radiation, which are necessary to achieve the therapeutic result, by keeping side effects at low levels.
Radiation therapy is a non-invasive treatment, whose side effects are associated with the areas of the chest that are irradiated. Therefore, we do not expect particular side effects for small peripheral tumors; however, for large tumors and when the mediastinum is irradiated due to lymphadenopathy, pneumonitis (described by dry cough) and esophagitis (described by difficult and painful swallowing) may appear. The side effects of radiation therapy are more frequent and greater when chemotherapy is concomitantly administered. The acute side effects of radiation therapy are usually treated shortly after its completion.
OUR APPROACH

As soon as you visit the Metropolitan Hospital Radiation Oncology Center, you will be approached by a dedicated team of specialists, who will tailor the treatment to your individual needs. Other than radiation oncologists, this specialized team includes: the medical physics department, which consists of radiophysicists who specialize in the latest radiation therapy technologies, radiologic technologists, nursing and secretarial staff. Our team also works closely with all the medical specialties involved in lung cancer, such as thoracic surgeons, pulmonary specialists and medical oncologists, but also radiologists, nuclear physicians, anatomic pathologists and molecular biologists. This guarantees the most individualized, modern and effective treatment, with the least possible side-effects.
The state-of-the-art radiotherapy techniques and the skills acquired by the doctors from their training in centers of excellence in Europe and the USA ensure highly accurate and targeted tumor treatment, by delivering the maximum radiation dose possible, with the least damage to healthy cells.
At Metropolitan Hospital we offer state-of-the-art radiation therapy techniques to treat lung cancer. These include:
- Three Dimensional Conformal Radiotherapy (3D-CRT): It is a technique that uses three dimensional CT images to design the treatment plan. As a result, the radiation fields are based on the exact shape of the targeted tumor and the least possible harm to neighboring healthy organs (see. fig.). This increases accuracy when targeting lung tumor and reduces the dose to the surrounding healthy tissue, compared to the older 2D radiotherapy techniques. In addition, it provides us with the opportunity to find out the exact dose received by each part of the lung tumor and the normal tissue, through the study of special diagrams (see. fig.) known as Dose Volume Histograms (DVH). This allows us to select the appropriate treatment plan offering the best coverage of the target volume, minimizing the radiation dose to normal organs. Specifically, we must make sure that the selected plan is associated with less than 10% mild side-effects and less than 0.5% severe side-effects.
- Intensity Modulated Radiotherapy (IMRT): It is an advanced type of highly accurate and targeted radiation therapy that is considered the next generation in 3D-CRT, used by most radiotherapy centers in Greece. As evident in the following image, IMRT further improves the possibility of adjusting the high radiation doses to the shape of the lung tumor, reducing the burden received by the healthy lung parenchyma and esophagus. This reduces the possibility of side-effects developing in these organs.
- Image Guided Radiotherapy (IGRT) and four-dimensional computed tomography (4D-CT): Other than respiration-induced tumor motion, lung tumors are also characterized depending on their localization.
TREATMENT
At the Metropolitan Hospital Radiation Oncology Department, we use advanced respiration-induced tumor motion recording techniques (Real-time Position Management System – RPM), while performing CT planning for radiation therapy (4D-CT). This technique allows the planning of all the tumor positions during respiration to include them in the radiation fields (minimizing any misses) (see image), or to irradiate the tumor during a specific phase of the breathing cycle (thus being able to reduce the extent of the radiotherapy fields (RPM Respiratory Gating System).
- • Finally, radiation therapy can be performed under image guidance (IGRT), namely controlling the patient’s position prior to the session and delivering the radiation, to ensure the precise and safe coverage of the target on a daily basis. In particular, we are able to perform three-dimensional imaging of the chest using a CT system integrated with linear accelerator (Cone Beam CT, Varian Trilogy®). Once images are taken, a comparison is made with the corresponding treatment plan images and any differences are automatically corrected with the correct movements of the treatment bed. Other than the patient’s position, three-dimensional imaging allows us to control the position, size and shape of the lung tumor (see image), thus allowing the early modification of the treatment in case any of these changes.
- Fusion of CT planning images with PET-CT images: This technique allows the radiation oncologist to precisely plan the lung tumor, especially when the tumor has obstructed a bronchus and it is difficult to distinguish it from induced atelectasis.
- Endobronchial Brachytherapy (HDR): In the case of brachytherapy, a radioactive source is inserted next to or into the lung cancer via the bronchi under image-guided bronchoscopy (radioscopy and/or computed tomography). This technique is primarily indicated to relieve the patient’s symptoms (mainly dyspnea), especially when the patient has been irradiated in the same area in the past. The sudden reduction of the dose at a small distance from the radioactive sources allows us to deliver a high dose of radiation to the tumor, while avoiding exposure to neighboring organs.