The prostate is a gland found only in men. It is walnut-sized, but grows with age. It encircles the upper part of the urethra immediately beneath the urinary bladder and is palpable with a digit exam.
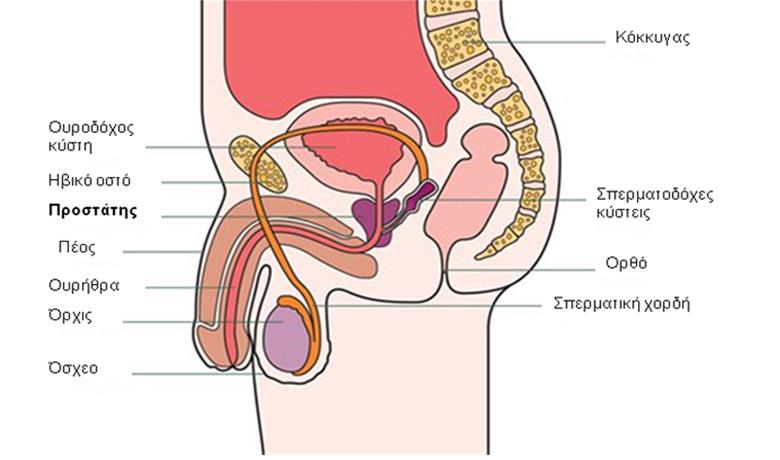
The prostate produces a milky, thick fluid which constitutes 20-30% of semen, along with the sperm produced by the testicles and the fluid in the seminal vesicles. It also produces a protein known as Prostate Specific Antigen (PSA), which liquefies semen.
The prostate is divided into two lobes and 4 zones (peripheral, central, transitional and anterior fibro-muscular zone) and it is surrounded by a fibromuscular band.
PROSTATE CANCER DEVELOPMENT
Prostate cancer develops in the glandular cells of the prostate gland. It is believed that cancer develops from existing precancerous lesions of the prostate cells known as prostatic intraepithelial neoplasia (PIN). In reality, most men already have PIN by the age of 50 years. With time, these cells acquire the ability to proliferate and in doing so create a tumor in the prostate gland. The majority of the tumors (70%) are detected in the peripheral zone of the prostate. Later, the tumor may have grown enough to penetrate neighboring organs, such as seminal vesicles, and finally acquire the ability to infiltrate vessels and spread to lymph nodes and remote sites.
EPIDEMIOLOGICAL DATA

Prostate cancer is the most frequently diagnosed cancer in Europe and the most common non-skin cancer among men. It is estimated that 2790 new prostate cancer cases were diagnosed in Greece in 2008.
The survival rates of prostate cancer patients are continuously rising as a result of public awareness, screening and significant advancements in prostate cancer treatments.
ETIOLOGICAL FACTORS

There are three well-documented risk factors for the development of prostate cancer: age, race/ethnicity (higher in African Americans) and pattern of inheritance.
Prostate cancer is extremely rare in men under 45 years, while the average age of diagnosis is 70 years. It is believed that 8 in 10 men aged 80 years and above have at least small prostate cancer foci, while most of these cancers develop very slowly and will never show symptoms.
Family history of prostate cancer in a first-degree relative multiplies that risk approximately 2-fold, and a family history of two first-degree relatives, gives rise to a 5- to 11-fold increased risk.
Lastly, certain studies have shown a correlation between the risk of prostate cancer and obesity, low vitamin D levels, the uptake of multivitamins for more than 7 times a week, the administration of statins (cholesterol reducing drugs) and high calcium uptake.
SYMPTOMS AND DIAGNOSIS

Men with early prostate cancer usually do not have symptoms given that these appear when the tumor is large enough to place pressure on the urethra. Nonetheless, in men over 50 years of age, the size of the prostate gland tends to increase because of a benign disorder known as benign prostatic hyperplasia. Thus, both hyperplasia and prostate cancer are accompanied by similar symptoms. These include:
- Urination difficulties
- Frequent urination, especially at night
- A burning sensation in the urethra during urination
- Blood in urine or semen (rare)
- Painful ejaculation
Prostate cancer screening should start at the age of 50 years and include a prostate specific antigen (PSA) test and digit exam. A prostate gland biopsy is the only examination that can confirm diagnosis. During biopsy, tissue samples are taken from both prostate lobes and sent for histological examination. Collection is done using a transrectal ultrasound guided prostate needle biopsy.
Disease aggressiveness is determined by the PSA value, the clinical stage of the cancer and the sum of the disease’s malignancy grades, known as the Gleason score, and arises from the prostate gland biopsy histological examination.
TREATMENT

Prostate cancer treatment consists of active surveillance, radical prostatectomy, radiation therapy and hormone therapy. Below we will refer to radiation therapy in conjunction with the two other prostate cancer treatment modalities (surgery and hormone therapy).
In the case of early prostate cancer, the patient can choose between radiation therapy and surgery with similar results. For larger, more aggressive tumors, radiation therapy is frequently combined with hormone therapy. Radiation therapy is also indicated after radical prostatectomy when the tumor has not been completely removed or when it relapses.
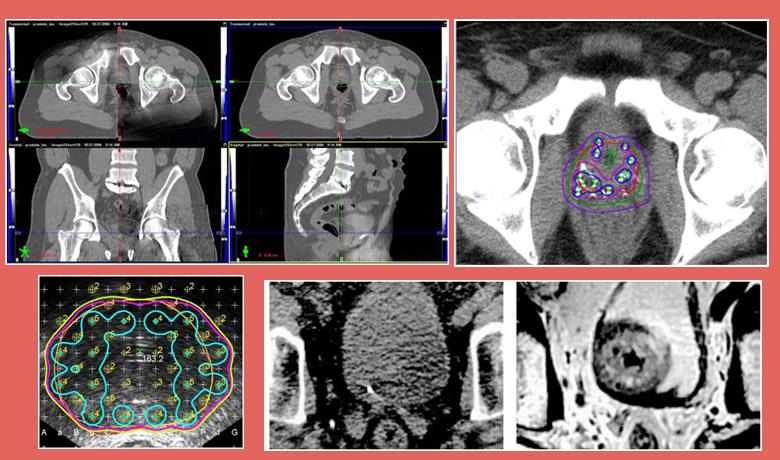
External beam radiation therapy uses high-energy X-rays (photons) to treat prostate cancer. The rays are produced by a linear accelerator, positioned at a distance from the patient’s body. Three Dimensional Conformal Radiotherapy (3D-CRT) is the most frequently used external beam radiation therapy technique, while Intensity Modulated Radiotherapy (IMRT), an improved version of 3D-CRT which focuses the dose on the target and avoids healthy tissues, has been increasingly gaining ground over recent years, especially in terms of treating prostate cancer.
RADIATION THERAPY

External beam radiation therapy is performed over a number of daily visits to our Center on an outpatient basis (without hospitalization).
The application of IMRT made using state-of-the-art and more precise image guided radiotherapy (IGRT) of the targeted area prior to the radiation therapy all the more necessary.
Brachytherapy is a form of radiation therapy in which a radioactive source irradiates the prostate from the inside. This can be achieved using two techniques. Either with permanent seed implantation (radioisotopes) in the prostate gland that cease irradiating 9-12 months after implantation into the patient’s body (LDR – Low Dose Rate Brachytherapy), or with the temporary placement of catheters, which are removed once treatment is completed (HDR – High Dose Rate Brachytherapy).
Well-designed studies have found that the larger the radiation therapy dose, the better prostate cancer is controlled. Similar studies have found that it is important to combine radiation therapy and hormone therapy in patients with intermediate and high-risk prostate cancer.
Contemporary radiation therapy techniques have managed to reduce prostate cancer treatment side effects to a minimum. Focusing on high-dose radiation on a tumor, with less impact on healthy organs thanks to IMRT, but also the safety that these doses will be precisely delivered to the target, thanks to IGRT, have established radiation therapy as extremely safe in prostate treatment. Thus, we are now able to deliver high doses of radiation, which are necessary to achieve the therapeutic result, by keeping side effects at low levels.
Radiation therapy is a non-invasive treatment that does not cause incontinence, maintains erectile function in the majority of cases and, by virtue of modern techniques, presents only a small rate of gastrointestinal (e.g. diarrhea) and urinary (e.g. frequent urination) side effects, which are minor and can be treated shortly after radiation therapy in completed.
OUR APPROACH
As soon as you visit the Metropolitan Hospital Radiation Oncology Center, you will be approached by a dedicated team of specialists, who will tailor the treatment to your individual needs. Other than radiation oncologists, this specialized team includes: the medical physics department, which consists of radiophysicists who specialize in the latest radiation therapy technologies, radiologic technologists, nursing and secretarial staff. Our team also works closely with all the medical specialties involved in prostate cancer, such as urologists, medical oncologists, but also radiologists and anatomic pathologists. This guarantees the most individualized, modern and effective treatment, with the least possible side-effects. This impeccable collaboration is further forged through the Hospital’s weekly Oncology Council meetings, with the participation of staff from all the relevant medical specialties.
The state-of-the-art radiotherapy techniques and the skills acquired by the doctors from their training in centers of excellence in Europe and the USA ensure highly accurate and targeted tumor treatment, by delivering the maximum radiation dose possible, with the least damage to healthy cells.
At Metropolitan Hospital we offer state-of-the-art radiation therapy techniques to treat prostate cancer. These include:
- Three Dimensional Conformal Radiotherapy (3D-CRT)
- Intensity Modulated Radiotherapy (IMRT)
- IMRT allows radiation oncologists to increase the dose being delivered to the prostate up to 86 Gy, while protecting neighboring healthy tissues. This is the only technique that allows the safe increase of the dose beyond 76 Gy with conventional fractionation or the increase of the dose with subfractionation (larger daily radiation doses).
- The Memorial Sloan-Kettering Cancer Center has the largest experience in this technique and to this day has published the results of high-dose radiation therapy using IMRT in two large series with more than 1000 patients [6, 7], reporting a disease control rate of 70% to 98% depending on the patients’ risk factors.
- Moreover, IMRT allows the delivery of high doses to clinically suspicious pelvic lymph nodes, while protecting the small intestine.
- Image Guided Radiotherapy (IGRT)
- Fusion of CT planning images with MRI or MRI Spectroscopy images
- Prostate Brachytherapy with the implantation of radioactive seeds (LDR) and temporary placement of catheters (HDR)