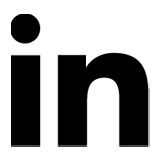
In the world of modern orthopedic surgery, the presence of a groundbreaking, portable intraoperative imaging system, such as the O‑Arm, marks a new milestone. This multidimensional system, combined with the surgical navigation system (Navigation), achieves 100 % accuracy in locating and managing even the most delicate orthopedic conditions of the spine.
This precision allows surgeries to be performed in anatomically challenging areas of the spine, minimizing the risk of medical error. Consequently, even highly complex procedures for conditions such as scoliosis, kyphosis, spondylolisthesis, or osteoporotic fractures become safer and more effective. At the same time, surgical time is significantly reduced (by up to 50 %), decreasing the overall operative burden—even for high-risk patients.
The O‑Arm system provides 3D imaging of tissues during surgery, offering greater safety and improved recovery prognosis.
Key applications of the Orthopedic Team:
- Minimally invasive spinal surgeries, performed with precision and speed
- Correction of deformities such as scoliosis and kyphosis in adults and children using robotic technology (ExcelsiusGPS) and navigation
- Management of degenerative diseases, spondylolisthesis, spinal stenosis, fractures, or spinal tumors
The Orthopedic Surgical Team is specialized in spinal conditions and has extensive experience in internationally recognized centers. They employ the latest techniques, including endoscopic and minimally invasive procedures, guided by advanced tools such as ExcelsiusGPS and O‑Arm II.
Advantages:
- Accuracy & Safety: thanks to O‑Arm II and robotic navigation technologies
- Faster Recovery: reduced surgical time, shorter hospitalization, and less patient burden
- Holistic Approach: in collaboration with neurologists, physiatrists, and physical therapists for complete rehabilitation
How the systems works
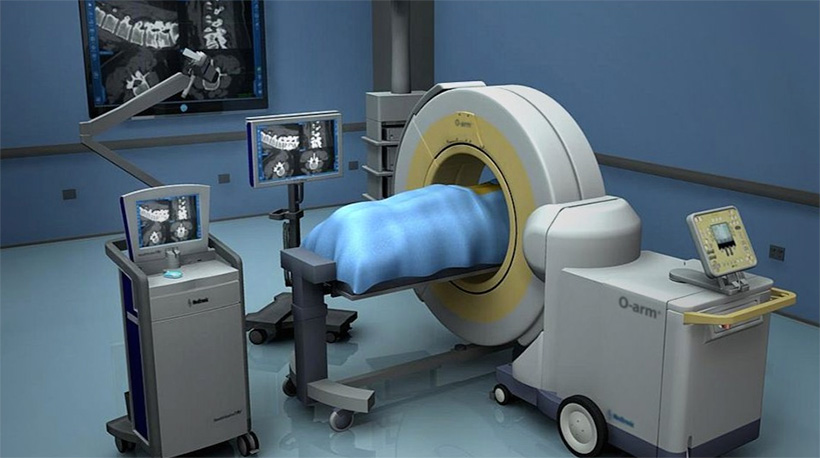
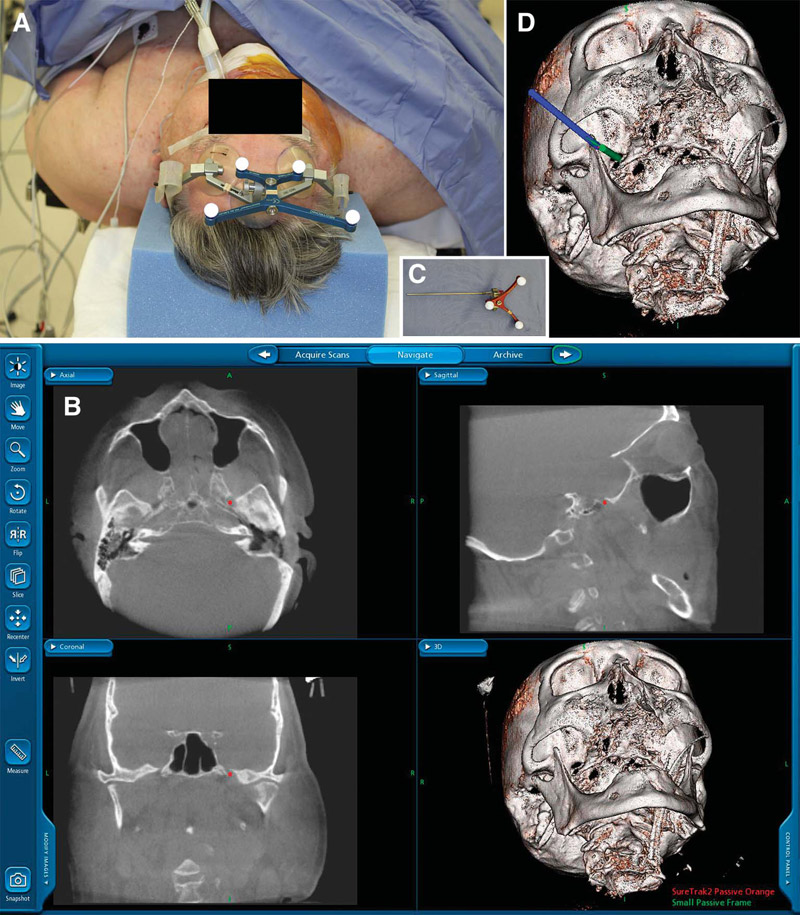
The system works as follows: just as satellites detect the position of a GPS unit in our car and the navigation system displays its location on current maps, a camera in the operating room tracks the position of surgical instruments. This position is displayed on the system’s screen, always in real time, in direct correlation with the patient’s actual anatomy (optical tracking technology).
In place of the camera, the system can use a transmitter. The transmitter generates an electromagnetic field around the patient, and anything that enters this field is automatically detected (electromagnetic tracking technology). Tiny sensors attached to the surgeon’s instruments are recognized within the field and provide continuous, highly accurate information about the position of the tools in relation to the patient’s anatomy.
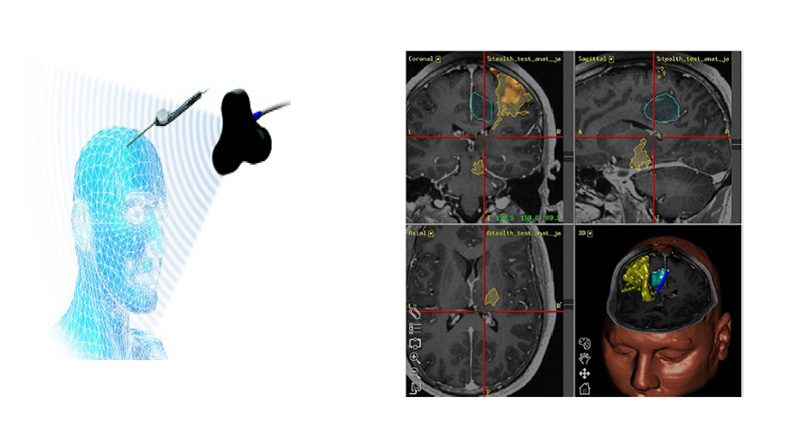
Surgical navigation systems are located in the operating theater and use either optical or electromagnetic tracking technology. They consist of the specialized camera or transmitter, the computing unit with its dedicated software, the display monitor, special navigation instruments, and adaptors that allow standard surgical tools to be recognized by the system.
The camera or transmitter identifies and tracks the position of moving instruments by cross-referencing the corresponding signals (sphere reflection in optical technology, signal coordinates in electromagnetic technology). The computing unit processes these signals, and their position is projected onto the system’s display. At this stage, the “map” is no longer a road atlas but instead a CT or MRI scan—or even a fusion of multiple imaging studies—providing surgeons with unparalleled precision during surgery.
Main applications
Modern surgical navigation systems provide an integrated methodology that includes imaging examinations (MRI, CT, MR angiography, CT angiography, ultrasound), preoperative planning, intraoperative navigation, and postoperative data archiving. Surgical navigation is primarily used in Neurosurgery, Orthopedics, and Otolaryngology.
Advances in surgical navigation technology have significantly contributed to the progress of Neurosurgery and are now internationally established as the method of choice for cranial procedures, replacing older frame-based stereotactic techniques.
The main applications in neurosurgery include:
- Removal of brain and spinal cord tumors (selection of craniotomy site, surgical trajectory and approach, tumor localization and delineation).
- Biopsy and catheter placement.
- Functional Neurosurgery (placement of electrodes for deep brain stimulation).
- Spinal Surgery
Navigation has rapidly expanded in recent years for spine procedures, as it provides intraoperative three-dimensional visualization of anatomy and enables precise localization of instruments and implants (e.g., screws) relative to the patient’s anatomy. This allows for detailed planning of the surgical approach and real-time visualization of screw placement.

Additionally, intraoperative navigation has recently been applied in musculoskeletal tumor surgery. We have used navigation in several cases for percutaneous ablation of osteoid osteomas or metastatic lesions, often combined with osteoplasty.
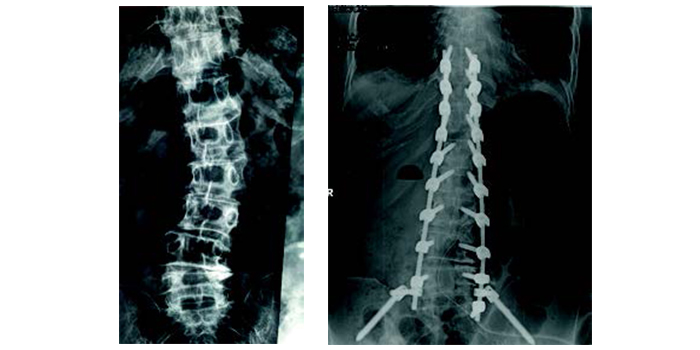
Scoliosis and Kyphosis
Intraoperative 3D Imaging & Surgical Navigation System:
For the first time in Greece, in 2016, the Metropolitan Hospital successfully implemented a 3D imaging and surgical navigation system for children with scoliosis.
The system enabled real-time placement of implants with CT-level accuracy. This precision virtually eliminates the risk of medical errors and permanent neurological damage, while also providing excellent aesthetic outcomes—particularly important for girls with scoliosis. The system is now used for both pediatric and adult patients with scoliosis or kyphosis.
Scoliosis and Kyphosis
The human spine has natural curves that help the body stand upright and remain flexible. Scoliosis is characterized by a twisting of the spine. It affects children, adolescents, and adults of both sexes. Idiopathic scoliosis is the most common form, affecting approximately 2% of the global population. Fortunately, only a small percentage of these cases require treatment. Kyphosis is an increase in the natural thoracic curve or a decrease in the normal lumbar curve. It usually affects older adults with osteoporosis, but adolescents can also be affected.
Causes
In most cases, the cause of scoliosis in children and adolescents is unknown, although it is believed to have a genetic background passed down through generations. Kyphosis in adolescents is often caused by Scheuermann’s disease, which can lead to pain. Adult scoliosis usually results from untreated childhood or adolescent scoliosis or from spinal aging. In adults, kyphosis is typically age-related, causing pain and difficulty in maintaining an upright posture.
Symptoms:
Parents may suspect scoliosis in a child or adolescent if one shoulder appears higher than the other or the pelvis seems tilted. Look for back deformities, usually in the shape of an “S” or “C.”

In adolescents with back pain and kyphosis, Scheuermann’s disease should be ruled out. In adults, a lateral shift of the body to the right or left may indicate scoliosis, especially if accompanied by pain.
Kyphosis is noticeable from the progressive “hunchback” appearance and the need to walk with bent knees. Pain is almost always present. Each child or adult with scoliosis or kyphosis is a unique case, and treatment must be individualized.
Management of Scoliosis / Kyphosis
Monitoring
Children and adolescents with mild scoliosis or kyphosis should be regularly monitored for potential progression as their body grows. Adults should be monitored if scoliosis or kyphosis is present but not associated with neurological problems. In the early stages, targeted physiotherapy and medication play a key role in reducing pain.
Bracing
For children and adolescents with moderate scoliosis, advances in materials have led to lighter and more “aesthetic” braces that are more easily accepted. Classic Boston braces, as well as newer dynamic or nighttime Providence braces, can be used depending on age, scoliosis type, and severity. Unfortunately, no type of brace can correct scoliosis in children or adolescents; their role is limited to halting curve progression. In adolescents with Scheuermann’s disease, braces may help halt progression, manage pain, and correct kyphosis. In adults, braces are less effective than in children.
Surgical Alternatives
For children and adolescents, surgical correction of scoliosis is recommended for curves exceeding 45 degrees. Without surgery, these curves may continue to worsen even after skeletal maturity, leading to chronic pain, respiratory dysfunction, and psychosocial effects, especially in girls. Once scoliosis exceeds 45 degrees, braces are no longer effective. For adolescents with Scheuermann’s kyphosis, surgery is indicated if the curve progresses to 70 degrees despite bracing and is associated with pain.
In adults, treatment is generally surgical. Minimally invasive procedures Advantages of Intraopecan help correct kyphosis and relieve pain from osteoporotic fractures. Adult scoliosis should be surgically corrected if associated with pain in the lower back or legs that limits daily activities and reduces quality of life.
Metropolitan Hospital: First Excelsius GPS™ in Greece
The Excelsius GPS™ system offers:
- 3D visualization of spinal anatomy, surgical tool movement, and implant placement with high precision
- Preoperative planning and implant selection
- Combination of surgical navigation and robotic guidance
- Minimization of risk to neural structures
- Shortened hospital stay
- Rapid return to full activity